
University of New South Wales Law Journal


|
Home
| Databases
| WorldLII
| Search
| Feedback
University of New South Wales Law Journal |

|
(FAILED) VOLUNTARY EUTHANASIA LAW REFORM IN AUSTRALIA: TWO DECADES OF TRENDS, MODELS AND POLITICS
LINDY WILLMOTT[*], BEN WHITE[**], CHRISTOPHER STACKPOOLE[***], KELLY PURSER[****] AND ANDREW MCGEE[*****]
Euthanasia remains a topical issue in Australia. Legislative attempts
to reform the law occur regularly. In 2013 alone, three Bills seeking to
legalise voluntary euthanasia (‘VE’) or physician-assisted suicide (‘PAS’) were introduced into different state parliaments;[1] and two issues and background papers were written to inform those debates.[2] In June 2014, the Australian Greens Senator and now leader of that party, Richard Di Natale, released an exposure draft of a Bill for consultation which would enable an Australian resident to receive assistance to die.[3] In May 2015, the Victorian Legislative Council directed the Standing Committee on Legal and Social Issues to report on the need for laws to allow citizens to make ‘end-of-life choices’ (a reference that is sufficiently broad to include VE and PAS). Most recently, in December 2015, Senator David Leyonhjelm from the Liberal Democratic Party introduced a Bill into the Senate seeking reform in this field.[4] VE and PAS also became a critical policy platform for political parties during the 2013 federal election.[5] Discussion of these issues remains prevalent in the media.[6] In part, this is fuelled by the not infrequent prosecutions of family members, friends and medical practitioners who have been involved with the death of persons who were terminally ill or who otherwise requested assistance to terminate their own life.[7]
This issue is also topical internationally, as we witness a trend towards the legalisation (or decriminalisation) of VE and PAS. There has been legislative reform in the Netherlands,[8] Belgium,[9] Luxembourg,[10] the United States (Oregon,[11] Washington,[12] Vermont[13] and California)[14] and in Canada (Quebec).[15] Assisting another to die is also lawful in Switzerland provided the assistance is not given for ‘selfish motives’.[16] Last year, the Canadian Supreme Court held unanimously that criminal law provisions prohibiting physician assistance in dying contravened rights conferred by the Canada Act 1982 (UK) c 11, schedule B part I (‘Canadian Charter of Rights and Freedoms’).[17] In some jurisdictions, such as in British Columbia in Canada[18] and the United Kingdom,[19] VE and PAS have been the subject of specific prosecutorial guidelines.
Within Australia, there have been many attempts to pass VE legislation. From 16 June 1993[20] until the date of writing, 51 Bills have been introduced into Australian parliaments dealing with legalising VE or PAS.[21] Despite these numerous attempts, the only successful Bill was the Rights of the Terminally Ill Act 1995 (NT) (‘ROTTIA’), which was enacted in the Northern Territory, but a short time later overturned by the controversial Euthanasia Laws Act 1997 (Cth). Yet, in stark contrast to the significant political opposition, for decades Australian public opinion has overwhelmingly supported law reform legalising VE or PAS.[22]
While there is ongoing debate in Australia, both through public discourse[23] and scholarly publications,[24] about the merits and dangers of reform in this field, there has been remarkably little analysis of the numerous legislative attempts to reform the law, and the context in which those reform attempts occurred. The aim of this article is to better understand the reform landscape in Australia over the past two decades. The information provided in this article will better equip Australians, both politicians and the general public, to have a more nuanced understanding of the political context in which the euthanasia debate has been and is occurring. It will also facilitate a more informed debate in the future. The article seeks to achieve this aim by considering two separate but related aspects of the reform attempts.
First, in Part III, the authors chart the many legislative attempts to reform the law over the previous two decades (including the circumstances surrounding the passage of the Northern Territory legislation and its demise when overturned by the Commonwealth Government), and the jurisdictions in which these reform attempts are occurring. Part III then considers some political dimensions of the debate including who has been proposing reform, relevant political affiliations and the role, more broadly, that party politics has played in the past and may play in the future. That Part also provides a detailed analysis of how far the Bills progressed through parliaments and how they were disposed of. Finally, through an analysis of parliamentary records, the authors have identified which Bills came close to passing, and comment on whether any conclusions can be drawn from the fact that these particular Bills had a greater level of political support.
The second way in which this article seeks to deepen understanding is through an in-depth examination of the 51 Bills. If there is to be legislative reform in Australia, there will and should be close scrutiny and debate about the details of the Bills. As we shall see in Part IV, there can be significant variation in the content of the legislative proposals which affects, in important ways, how the regimes would operate. Decisions made about the content of the Bill will affect issues such as eligibility criteria (restricted to adults with capacity who are terminally ill and seek assistance to die, or available to a broader cohort), safeguards (involvement of treating doctor only, or should other specialists be involved), and state oversight (should each death be independently reviewed to ensure compliance with the regime, and should such review be prospective or retrospective). Yet, to date, there has not been a comprehensive analysis of how the Australian Bills have dealt with these and other issues. We do not know whether there has been general consensus or diversity on these and other critical points in the Bills to date. A consensus in some areas but variation in others, if this is the case, may signal the issues on which there might be particular focus when these Bills are debated in future years. Part IV analyses in detail the various legislative models and notes those areas of convergence and divergence. In this analysis, particular mention is made of the features of the Bills identified in Part III as ‘close to passing’. In Part V, the authors make some concluding remarks about the Australian reform experience to date, and speculate about the implications that this may have for reform attempts in the future.
We begin, however, in Part II, by defining frequently used terms. In this debate, people can be at cross-purposes because of different understandings of the same term. It is important to clarify what we mean in this article when we use various terms.
Both in Australia and overseas, the VE and PAS debates have been undermined by semantic ambiguity. We therefore seek to clarify what we mean when we refer to the terms included in the table below.[25]
Table 1: Terminology
|
Term
|
Meaning
|
Example
|
|---|---|---|
|
Euthanasia
|
For the purpose of relieving suffering, a person performs a lethal
action[26] with the intention of
ending the life of another person
|
A doctor injects a patient with a lethal substance to relieve that person
from unbearable physical pain
|
|
Voluntary euthanasia (‘VE’)
|
Euthanasia is performed at the request of the person whose life is ended,
and that person is competent
|
A doctor injects a competent patient, at their request, with a lethal
substance to relieve that person from unbearable physical pain
|
|
Competent
|
A person is competent if he or she is able to understand the nature and
consequences of a decision, and can retain, believe, evaluate,
and weigh
relevant information in making that decision
|
|
|
Non-voluntary euthanasia
|
Euthanasia is performed and the person is not competent
|
A doctor injects a patient in a post-coma unresponsive state (sometimes
referred to as a persistent vegetative state) with a lethal
substance
|
|
Involuntary euthanasia
|
Euthanasia is performed and the person is competent but has not expressed
the wish to die or has expressed a wish that he or she does
not die
|
A doctor injects a competent patient who is in the terminal stage of a
terminal illness such as cancer with a lethal substance without
that
person’s request
|
|
Withholding or withdrawing life-sustaining
treatment[27]
|
Treatment that is necessary to keep a person alive is not provided or is
stopped
|
Withdrawing treatment: A patient with profound brain damage as a
result of a heart attack is in intensive care and breathing with the assistance
of a ventilator, and a decision is made to take him or her off the ventilator
because there is no prospect of recovery
Withholding treatment: A decision is made not to provide nutrition
and hydration artificially (such as through a tube inserted into the stomach)
to
a person with advanced dementia who is no longer able to take food or hydration
orally
|
|
Assisted suicide
|
A competent person dies after being provided by another with the means or
knowledge to kill him- or herself
|
A friend or relative obtains a lethal substance (such as Nembutal) and
provides it to another to take
|
|
Physician-assisted suicide (‘PAS’)
|
Assisted suicide where a doctor acts as the assistant
|
A doctor provides a person with a prescription to obtain a lethal dose of a
substance
|
This Part of the article analyses the many attempts to reform euthanasia law in Australia’s states and territories. It commences with a detailed consideration of the first attempts to introduce VE laws and the circumstances surrounding the enactment of the Northern Territory legislation and its overturn, and then provides an overview of all reform attempts in Australia. Importantly, this Part extends beyond a description of the legislative attempts and unpacks some of the politics associated with the euthanasia reform efforts: political affiliations of proponents, voting trends of members of parliament (along party lines or not) and, more generally, the role politics has played in euthanasia reform in Australia. Next, this Part charts how far the various Bills progressed, and identifies seven Bills that garnered the most political traction. Based on identification and analysis of these seven Bills, this Part concludes with some observations and speculation about what factors may be influential in achieving reform.
The first VE Bill introduced into any Australian parliament was the Voluntary and Natural Death Bill 1993 (ACT). The Bill was introduced into
the Legislative Assembly of the Australian Capital Territory by Michael
Moore (independent) on 16 June 1993.[28] The Bill was designed to achieve three purposes: (a) to facilitate VE in limited circumstances;[29] (b) to permit a doctor to withhold or withdraw treatment in limited circumstances;[30] and (c) to enable a person to give a direction about future treatment to operate when that person becomes incompetent.[31] When the Bill was introduced, the matter was referred to the Select Committee on Euthanasia, chaired by Michael Moore, whose report was tabled in Parliament on 14 April 1994.[32] The Select Committee concluded that it would not be appropriate[33] and politically inopportune[34] to pass legislation to allow for VE, and the Bill was discharged from the notice paper by Michael Moore on 11 May 1994[35] prior to the 1995 election.[36] In coming years, Michael Moore would introduce into the Legislative Assembly four further Bills to legalise or decriminalise euthanasia.[37]
On 22 February 1995, soon after the discharge of the Voluntary and Natural Death Bill 1993 (ACT), the Chief Minister of the Northern Territory, Marshall Perron,[38] tabled a private member’s Bill to legalise VE and PAS.[39] On the same day, that Bill was referred to a Northern Territory Select Committee on Euthanasia for consideration.[40] The report of the Committee, which was tabled in May 1995, provided no specific recommendations regarding whether legislation permitting VE should be introduced, although it recommended amendments to the initial Bill.[41] On 24 May 1995, Marshall Perron resigned as Chief Minister, indicating that he did not want his position to influence the manner in which the members of his party voted. After extensive debate, the Assembly divided and on a vote of 13:12, the Bill passed the second reading stage.[42] After a debate extending into the early morning of 25 May 1995, the Bill passed the committee stage and third reading on a vote of 15:10.[43] With the enactment of the ROTTIA, the Northern Territory became the first, and only, jurisdiction within Australia to introduce legislation for VE. It also became the first jurisdiction in the world to establish a legislative regime that permitted the practice.
However, the ROTTIA did not last long on the statute book. On 9 September 1996, Liberal Party member, Kevin Andrews, introduced into the Commonwealth Parliament the controversial Euthanasia Laws Bill 1996 (Cth) which sought to amend the territories’ Self-Government Acts[44] to deprive them of their capacity to pass VE or PAS legislation.[45] Despite serious remonstrations by the Northern Territory and the Australian Capital Territory Governments, on
9 December 1996, the Euthanasia Laws Bill 1996 (Cth) passed the second reading stage 90:39,[46] and passed the committee and third reading stages with a resounding 88:35 majority.[47] The Bill was introduced into the Senate on
12 December 1996 by Senator John Herron of the Liberal Party.[48] On 24 March 1997, the Bill passed the second reading[49] and third reading stages without amendment 38:33.[50] The Euthanasia Laws Act 1997 (Cth) came into effect on
27 March 1997,[51] amending the territory Self-Government Acts and dismantling the ROTTIA. Since the passage of the Euthanasia Laws Act 1997 (Cth), there have been six unsuccessful attempts by members of the Australian Democrats[52] and Australian Greens[53] to remove the limitation on the legislative power of the territories. Most recently, in December 2015, a member of the Liberal Democratic Party introduced a Bill into the Senate seeking to do the same.[54]
There have been 51 Bills introduced into the various Australian parliaments since 1993. The names of these Bills, when, where and by whom they were introduced are listed in the Appendix. Seven of these Bills sought to remove the prohibition on territories legislating in this area and a further five sought to hold a referendum on law reform. The remaining 39 Bills proposed a model for law reform permitting VE and/or PAS.
Figure 1 provides a graphic illustration of the number of these VE Bills introduced and the year of their introduction.
Figure 1: Number of VE/PAS Bills Introduced into Australian Parliaments
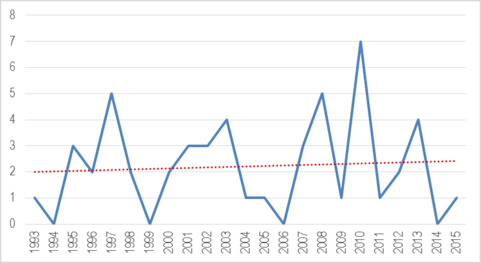
As demonstrated by the trendline,[55] the number of Bills introduced has been progressively increasing. The increasing trend is significant having regard to the fact that, since 1997, no Australian territory has been able to introduce a VE Bill due to the effect of the Euthanasia Laws Act 1997 (Cth). Furthermore, between 1993 and 1997, the Northern Territory and the Australian Capital Territory introduced two and five VE Bills respectively into parliament, in contrast to the states’ and Commonwealth’s average of 0.67[56] Bills per jurisdiction over this same five-year period. The territories, rather than the states, were more active in introducing VE initiatives prior to the Euthanasia Laws Act 1997 (Cth). Indeed, the significant decline in the number of Bills introduced between 1998 and 1999 directly correlates with the reduction in legislative attempts in the territories’ parliaments. Since 1998, the states and the Commonwealth have assumed a more active role in introducing an average of 2.22 Bills each year.[57] Since 2007, the average has increased to 2.7 Bills each year across Australia.[58] South Australia (20), New South Wales (8) and Western Australia (6) have led the states in introducing VE Bills. Tasmania has introduced two VE Bills, Victoria has only introduced one Bill, and Queensland is the only jurisdiction never to have introduced a VE or PAS Bill. There have been seven attempts at a federal level to abolish the Euthanasia Laws Act 1997 (Cth).
The politics of euthanasia law reform – in particular, the extent to which euthanasia has been a political issue and the reason that this has (or has not) been the case – has received remarkably little attention in the Australian literature.[59] This article does not aim to fill that gap in the literature, but in this section, we provide information about the political positions taken (or not taken) by Australian political parties, as well as the political affiliations of those members of parliament who have proposed reform. We provide an analysis of some of the voting patterns that have occurred, and make some observations about the political nature of the debate in Australia and the implications of this on the likelihood of reform.
Despite the ongoing and sustained media attention on VE and public support for reform, the largest political parties in Australia, the Liberal Party, the Australian Labor Party and the National Party, have not developed policy positions on the topic. This is in stark contrast to other parties that have deemed this to be an issue that should not be ignored. The Australian Greens have consistently supported VE since the party was formed in 1992, its policy being in favour of allowing terminally ill patients to seek assistance to die from their doctor.[60] Historically, the Australian Democrats have also supported reform of the law,[61] and more recently, the Australian Sex Party and the Liberal Democratic Party. Both the Christian Democratic Party and the Family First Party have adopted a position at the other end of the spectrum, and are strongly opposed to legalising VE.
The table below provides a breakdown of the VE Bills by affiliation of the proponent to a political party, if any, as well as by jurisdiction.
Table 2: Voluntary Euthanasia Bills by Political Affiliation of Proponent and Jurisdiction
|
|
Cth
|
ACT
|
NSW
|
NT
|
SA
|
Tas
|
Vic
|
WA
|
Total
|
|
Number of Bills introduced
|
7
(14%)
|
5
(10%)
|
8
(16%)
|
2
(4%)
|
20
(39%)
|
2
(4%)
|
1
(2%)
|
6
(12%)
|
51
(100%)
|
|
Political Affiliation of Proponent
|
|||||||||
|
Independent
|
0
|
5
|
0
|
0
|
11
|
0
|
0
|
0
|
16
(31%)
|
|
Australian Democrats
|
1
|
0
|
1
|
0
|
3
|
0
|
0
|
4
|
9
(18%)
|
|
Australian Greens
|
5
|
0
|
7
|
0
|
2
|
1
|
1
|
2
|
18
(35%)
|
|
Australian Labor Party
|
0
|
0
|
0
|
1
|
4
|
0
|
0
|
0
|
5
(10%)
|
|
Country Liberal
|
0
|
0
|
0
|
1
|
0
|
0
|
0
|
0
|
1
(2%)
|
|
Liberal Democratic Party
|
1
|
0
|
0
|
0
|
0
|
0
|
0
|
0
|
1
(2%)
|
|
Australian Greens –Australian Labor Party Joint Bill
|
0
|
0
|
0
|
0
|
0
|
1
|
0
|
0
|
1
(2%)
|
|
* All VE Bills introduced into Australian parliaments have been private
members’ Bills.
|
|||||||||
As can be seen, the independents and the members of the Australian Greens and the Australian Democrats have been the major proponents of VE reform. The Australian Greens introduced their first VE Bill in 2001 in New South Wales, and have accounted for 37 per cent of all VE Bills introduced in parliaments across Australia,[62] while the Australian Democrats have introduced 18 per cent. Independent members have been responsible for the introduction of 31 per cent of VE Bills. While this might seem significant, all independent VE Bills have been introduced by only two individuals, Michael Moore and Dr Bob Such. Indeed, it would seem that VE has primarily been the responsibility of individual members of parliament, with only 21 individuals having introduced all 51 Bills over the past 20 years. Only six Bills have been introduced by Australian Labor Party members.[63] Significantly, only one Bill has been introduced by a member of a conservative political party, Marshall Perron, when he introduced the ROTTIA, the only Bill within Australia to have been successfully enacted.
Regardless of whether a political party has developed a policy position on VE or, if one has been developed, the stance taken, all parties have universally allowed conscience votes on the matter of VE. Nevertheless, there appears to be a strong correlation between party affiliation and voting preferences, and indeed, many decisions are determined virtually according to the chosen party lines.[64] For example, in relation to the Euthanasia Referendum Bill 1997 (ACT), every Australian Labor Party member voted against the Bill, and every Liberal Party member (except one) voted against the Bill.[65] Similarly, every Liberal and Australian Labor Party member voted against the Crimes (Assisted Suicide) Bill 1997 (ACT), a Bill that significantly mitigated penalties for medical practitioners engaging in VE, while every Australian Greens member supported the Bill.[66] Similarly, when the Voluntary Euthanasia Trial (Referendum) Bill 2003 (NSW) was introduced, every Australian Greens and Australian Democrat member voted in favour of the Bill, and every member from the Liberal and Labor Parties voted against the Bill.[67] The same occurred when voting on the Voluntary Euthanasia Referendum Bill 1997 (NSW).[68] Furthermore, in both the Voluntary Assisted Dying Bill 2013 (Tas) and the Rights of the Terminally Ill Bill 2013 (NSW), all members of the Liberal Party voted against the proposed VE regimes.[69] In recent times, Australian Labor Party members are more likely to have an even distribution of votes, but the tendency has continued for members of conservative political parties to vote against VE Bills.[70]
The apparent influence of political allegiances on voting practices raises the broader question of what role politics currently plays in euthanasia law reform in Australia, and will play in the future. As evident from the above, a range of political coalitions have formed. The most common coalition (in favour of VE reform) is the Australian Greens and Democrats, frequently supported by sympathetic independents. Parties with direct religious affiliations forming the foundation of their policies, such as the Family First and Christian Democratic Parties, have universally opposed the passage of VE legislation. While the Liberal and Australian Labor Parties allow conscience votes, Liberal Party members are more likely to oppose VE, and Australian Labor Party members are more likely to have an even distribution.
The role that politics will play in future attempts to reform euthanasia in Australia is an interesting question in a country where the major political parties are secular and whose policy positions are, for the most part, not born of religious influence. As we have seen, the Liberal, Labor and National Parties do not have a formal position on euthanasia, so this issue is not one in which any of these parties can differentiate themselves from one another in the electorate. It is likely that none of these parties perceive that any political advantage will be gained by making euthanasia law reform a political issue.[71] While the Christian Democratic Party has a policy that stems from its religious philosophy, it is a minor political party which currently lacks political influence.
The Australian political landscape can be contrasted with countries such as the Netherlands and Belgium where there are more political parties, frequent (and varied) coalitions are negotiated to form government and parties can be divided along secular and non-secular lines. In such environments, having an articulated position (either for or against) euthanasia provides a point of differentiation, so can be a basis upon which voters can choose one party over another. It was this secular–non-secular divide that was influential in euthanasia becoming a political issue in both the Netherlands and Belgium.[72]
Although historically, religiously based parties have had little, if any, political influence in Australia, in the current political climate, minor parties have had a great deal more influence in some jurisdictions than has ever been the case.[73] This fact, combined with the political alliances that have already formed in Australia on this issue, may mean there is an increased likelihood for euthanasia reform to become a political issue in the future. This is certainly consistent with other indicators. For example, ‘euthanasia’ is raised as a political issue on ‘Vote Compass’, an online tool that has been increasingly used and promoted in the lead-up to elections, to assist the voting public to analyse political positions of the parties. Further, position statements on the topic are emerging not only from political parties but also from some peak groups,[74] possibly an indicator that this is an issue upon which it is no longer possible or appropriate not to have a position. These developments, of course, occur against the backdrop of regular and ongoing opinion polls that reveal sustained public support for reform.
Having considered some of the political aspects of the euthanasia debate, including the political affiliations of members introducing the Bills into parliament and some of the voting patterns that have emerged, it is instructive to examine in more detail how far in the parliamentary process the Bills reached, and how they were disposed of. For law reform to occur, it is not enough to have a proponent for change. The relevant parliament must be prepared to allocate time for the Bill to be considered and debated. If a high proportion of Bills remain as notices of motion without being introduced into parliament, for example, that signals less of an appetite for reform than if they all reached the second (or third) reading stage and were debated in full. As evident from the analysis below, the 50 Bills[75] that have been introduced over the past two decades have had varying degrees of progress through and consideration by their respective parliaments. In this section, we identify the stage that all of the Bills reached and how they were disposed of, that is by being passed, withdrawn, discharged or defeated, or by lapsing.
Table 3 provides a summary of the stage that the Bills reached and the disposition of the various Bills, broken up by jurisdiction.
Table 3: Summary of the Stage Reached and Disposition of Australian Voluntary Euthanasia Bills
|
|
Cth
|
ACT
|
NSW
|
NT
|
SA
|
Tas
|
Vic
|
WA
|
Total
|
|---|---|---|---|---|---|---|---|---|---|
|
Number of Bills introduced
|
6
(12%)
|
5
(10%)
|
8
(16%)
|
2
(4%)
|
20
(40%)
|
2
(4%)
|
1
(2%)
|
6
(12%)
|
50
(100%)
|
|
Stage Bill Attained in Parliamentary
Process[76]
|
|||||||||
|
Not introduced
|
0
|
0
|
4
|
0
|
0
|
0
|
0
|
0
|
4
(8%)
|
|
First reading
|
0
|
1
|
1
|
0
|
0
|
0
|
0
|
0
|
2
(4%)
|
|
Second reading
|
6
|
4
|
3
|
1
|
15
|
2
|
1
|
6
|
38 (76%)
|
|
Committee stage/ third reading
|
0
|
0
|
0
|
0
|
5
|
0
|
0
|
0
|
5 (10%)
|
|
Passed both houses
|
0
|
0
|
0
|
1
|
0
|
0
|
0
|
0
|
1
(2%)
|
|
Disposition of Bills
|
|||||||||
|
Discharged
|
1
|
2
|
0
|
0
|
1
|
0
|
0
|
0
|
4
(8%)
|
|
Withdrawn
|
0
|
0
|
2
|
0
|
0
|
0
|
0
|
0
|
2
(4%)
|
|
Lapsed
|
5
|
0
|
2
|
0
|
14
|
0
|
0
|
5
|
26 (52%)
|
|
Defeated
|
0
|
3
|
3
|
1
|
5
|
2
|
1
|
1
|
16 (32%)
|
|
Passed
|
0
|
0
|
0
|
1
|
0
|
0
|
0
|
0
|
1
(2%)
|
As can be seen from Table 3, a high majority of the Bills (88 per cent) reached at least the second reading stage, with only 8 per cent failing to be introduced into parliament. While 88 per cent of Bills reached the second reading stage, only 12 per cent passed that stage. In this section, we consider the various stages reached by the VE Bills against the backdrop of the historical purposes of the various parliamentary phases.
The purpose of the first reading stage is to enable the relevant chamber of parliament to inform itself of the nature and content of the Bill.[77] Parliamentary practice prescribes that the first reading stage is a purely formal procedure and one in which Bills are ordinarily passed without opposition.[78] The Voluntary Euthanasia Referendum Bill 1997 (NSW), introduced by Elisabeth Kirkby on 15 May 1997, is the only VE Bill that was defeated at the first reading stage.
The second reading stage is the most important element of the legislative process. Its purpose is to debate the principle of the Bill, rather than individual clauses.[79] Accordingly, Bills containing technical defects or limitations capable of rectification by reasoned amendment should be permitted to progress to the committee or consideration in detail stages, at which time closer scrutiny can be given to any technical issues. For this reason, some parliamentary speakers have ruled it impermissible for members to discuss a Bill by debating each individual clause. Instead, it has been ruled that the second reading debate should be confined to the objectives and foundation of the legislative proposal.[80]
Despite 88 per cent of Bills (44 Bills) reaching the second reading stage, all but one of those Bills did not progress any further. Having regard to the purpose of the second reading stage, this suggests that it is the efficacy or justifiability of VE at a policy level that is the problem, rather than the perceived inadequacy of the framework or procedural safeguards contained within the relevant legislative proposals. If the majority of politicians supported the principle of VE, but objected to the procedural safeguards or regulatory framework of the proposed legislation, a larger number of Bills would be expected to pass the second reading stage, though possibly fail during the consideration in detail stage.
The consideration in detail stage involves a rigorous and detailed analysis of the specific provisions, procedures, and mechanisms of the legislative proposal.[81] The applicable standing rules and orders often provide for the consideration of each provision of the Bill in order to ensure that all provisions are properly scrutinised and evaluated, and prohibit any amendments which would negative or undermine the purpose of the Bill.[82] This is because the relevant chamber of parliament has already assented to the underlying principle of the Bill during the second reading stage, and any further debate of the objectives of the Bill would be unnecessarily duplicative, constitute a collateral attack on the previous division, and subvert the function of the consideration in detail stage. Only
12 per cent of VE Bills have reached the consideration in detail stage. Accordingly, 88 per cent of VE Bills have not been subject to a detailed
analysis of their specific clauses. Therefore, the common arguments that VE Bills lack adequate procedural safeguards, or that euthanasia cannot be safely regulated, present presumptive conclusions that often have not been adequately tested or examined by the relevant chamber of parliament.
Once introduced into parliament, and regardless of the parliamentary stage reached, there was significant variation in how the Bills were disposed of. More than half (52 per cent) of Bills lapsed, 12 per cent were discharged or withdrawn, and only 32 per cent were defeated.[83] A Bill is defeated when a division is called and a vote taken. Of interest, however, is that many of the Bills were not disposed of in this fashion. In the sections that follow, we consider circumstances in which VE Bills were discharged, withdrawn or, as is most commonly the case, lapsed.
Six of the 50 VE Bills (12 per cent) have been either discharged (4 Bills or
8 per cent) or withdrawn (2 Bills or 4 per cent). Although this is not a large number, it is worth attempting to understand why 12 per cent of VE Bills were terminated in this way rather than by being defeated or lapsing. A Bill is ‘discharged’ when it has been formally presented to parliament and is subsequently removed from the notice paper.[84] A Bill is ‘withdrawn’ when the sponsor of the Bill has recorded a notice of intention to present the legislative proposal in the notice paper and subsequently removes the notification from the notice paper prior to the first reading.[85] In each Australian jurisdiction, it is the sponsor of the Bill who most commonly is responsible for the discharge or withdrawal of the Bill.[86]
A Bill is generally withdrawn or discharged for one of the following reasons: an equivalent Bill is proceeding through another chamber of the parliament; the Bill possesses latent substantive defects which may impede its passage through parliament; the Bill is procedurally or formally noncompliant with an applicable standing rule or order; the Bill has no reasonable prospect for success; or it is considered that keeping the Bill on the notice paper is politically inconvenient.
It is difficult to obtain direct evidence on why a Bill is discharged or withdrawn by its sponsoring member. Possibly the prevailing sociopolitical circumstances and the relatively controversial nature of VE Bills may explain why some VE Bills are terminated in this way. Putting aside one New South Wales Bill,[87] the mean period in which the remaining five VE Bills were discharged or withdrawn was 249 days, or approximately eight months, from an election. In each instance, the election date was reasonably foreseeable at the time of discharge or withdrawal as it was held towards the end of the three- or four-year prescribed legislative term for the relevant jurisdiction. The fact that VE Bills were discharged or withdrawn on average within eight months of a reasonably foreseeable election date may suggest a perception among certain parliamentarians that VE Bills are politically undesirable policies to be associated with during an election campaign.
The dissolution or prorogation of parliament causes all proceedings to conclude and any outstanding Bills on the notice paper to lapse regardless of their stage of progression.[88] As more than half the VE Bills (26 Bills or
52 per cent) are disposed of by lapsing, it is important to explore why this might be the case. The authors suggest that this occurs as a result of two, integrally related, issues: the lack of appetite of the three major political parties to debate the issue; and the relatively limited amount of parliamentary time devoted to private members’ Bills.
A private member’s Bill is one that is advanced by a member of parliament which has not officially been introduced by the government.[89] All Bills introduced by independent politicians or the opposition are private members’ Bills unless formally adopted by the government. Even Bills introduced by ministers of the incumbent government will be private members’ Bills where they are not submitted as part of government business. Under the Australian Westminster parliamentary system, the majority of time in parliament is allocated to considering government business. As explained in the House of Representatives Practice handbook:
The increasing need for Governments to control House time, assisted by the growth of strong party loyalty, led to a steady curtailment of opportunities for private Members to initiate bills and motions, and procedures to expedite the consideration of government business.[90]
Although procedural changes have resulted in more time being allocated to private members’ business, it remains substantially constrained by the political and temporal exigencies of the relevant chamber of parliament.[91] For example, between 1990 and 2014, only 8.3 per cent of time within the Commonwealth House of Representatives was assigned to private members’ business, which includes legislation and motions.[92]
Private members’ motions and petitions are often limited to the private members’ business period in the chamber of parliament which, in some jurisdictions, is not assigned separate time periods from that allocated to committee and delegation business.[93] Furthermore, in many jurisdictions, private members’ motions and petitions are not heard in the order of submission, but in an order determined by a selection committee which prioritises private members’ business.[94] Finally, private members’ Bills are frequently referred to advisory committees for consideration, which further delays the progress of the Bill through parliament.
The reluctance of the three major political parties to engage with the contentious issue of VE was considered in Part III(C). As these political parties are in government in all jurisdictions, the above practices and protocols enable governments to dictate the parliamentary agenda which, as evidenced in Table 3, has resulted in many of the VE Bills lapsing.
The practical impediments that can be encountered by the proponents of reform are illustrated by considering the procedural history of the Voluntary Euthanasia Bill 1996 (SA). The Bill was introduced into the South Australian Legislative Council on 6 November 1996 by a member of the Australian Labor Party, Anne Levy. However, as a result of frequent and protracted adjournments, the division for the second reading was not called until eight months later on 9 July 1997. On the same date, the Bill was moved for consideration by a select committee. Sandra Kanck, leader of the Australian Democrats, questioned the legitimacy of the referral of the Bill to a select committee, stating that:
I am not sure how much a select committee will achieve. We all know that the committee will disappear when the election is called, so I query its usefulness other than as a ploy to stop its becoming a controversial issue at the election. Nevertheless, I will support the committee.[95]
The Bill was referred to the Select Committee on 9 July 1997 and, after convening only twice, the Bill lapsed when Parliament was prorogued before the general election held on 11 October 1997. Despite the lapsing of the Bill, on 25 February 1998, Carolyn Pickles, leader of the Australian Labor Party in opposition, moved for the Social Development Committee to consider the Voluntary Euthanasia Bill 1996 (SA). The Bill was not reintroduced, and the report of the Social Development Committee that was tabled on 20 October 1999 recommended against the reintroduction of the Bill.
In this section of the article, we take the analysis of reform attempts one step further. We seek first to identify those Bills that came ‘close to passing’. If Bills in a jurisdiction are regularly being narrowly defeated after a considered debate in parliament, this may suggest law reform is imminent in that jurisdiction. The opposite will be the case if there is consistently so little support for the Bill in the house that they are generally disposed of without division. Second, we consider whether identifying Bills that were ‘close to passing’ sheds any light on the circumstances or environment in which it is more likely that reform will occur, or at least be seriously debated.
The process of identifying Bills that were ‘close to passing’ was an exacting and time-consuming task. A detailed investigation into each of the 50 Bills[96] was undertaken to determine whether the particular Bill was debated in parliament and, if so, whether a division was called to determine support for the Bill. The criterion to assess whether a Bill was ‘close to passing’ is necessarily subjective in nature, but that chosen by the authors was as follows: the Bill was supported by at least 70 per cent of the number of members required to pass the Bill through the house.[97]
As a result, the following Bills did not satisfy this criterion:
• Bills that were not introduced to parliament;
• Bills that were discharged or withdrawn without being debated;
• Bills that lapsed without being debated; and
• Bills that were debated but were defeated on the voices, or for which no division was called, or where less than 70 per cent of the support needed to pass the Bill was received.
Using this method, only 7 of the 50 Bills that have been proposed were ‘close to passing’. Table 4 below lists these Bills, the proponent and party affiliation (if any), the jurisdiction, how the Bill was disposed of, and the numbers that supported and opposed the Bill.
Table 4: Summary of the Australian Voluntary Euthanasia Bills ‘Close to Passing’
|
Title
|
Name
|
Affiliation
|
Jurisdiction
|
Status
|
Support
|
Oppose
|
|
Rights of the Terminally Ill Bill
1995[98]
|
Marshall Perron
|
Country Liberal
|
NT
|
Passed
|
15
|
10
|
|
Voluntary Euthanasia Bill 1996
|
Anne Levy
|
Australian Labor Party
|
SA
|
Lapsed[99]
|
12
|
8
|
|
Dying in Dignity Bill 2001
|
Sandra Kanck
|
Australian Democrats
|
SA
|
Lapsed[100]
|
10
|
9
|
|
Mark Parnell
|
Australian Greens
|
SA
|
Defeated
|
9
|
11
|
|
|
Dying in Dignity Bill 2002
|
Sandra Kanck
|
Australian Democrats
|
SA
|
Defeated
|
8
|
13
|
|
Bob Such
|
Independent
|
SA
|
Defeated
|
20
|
22
|
|
|
Voluntary Assisted Dying Bill 2013
|
Larissa Giddings and Nicholas McKim
|
Australian Greens–Australian Labor Party joint Bill
|
Tas
|
Defeated
|
11
|
13
|
Some observations can be made from this analysis. The first is to note that reform of the law governing VE is difficult. Of all the attempts over the past two decades, only one Bill was successful and only six others were ‘close to passing’. These seven Bills represent only 14 per cent of all attempts. This is perhaps a surprising outcome, especially in light of a high level of community support for the enactment of legislation.[101] The second observation is that there is nothing particularly remarkable about those Bills that were closer to passing than the
43 Bills that did not satisfy the criterion. There were no particular features that these Bills possessed which, as a group, distinguished them from the Bills that were not ‘close to passing’.[102] Third, these seven Bills are not all recent, nor does there seem to be a trend for the more recent Bills (those passed between 2010 and 2014) to be ‘closer to passing’. Of the 14 Bills that were introduced over the past five years, only two were in this group of ‘close to passing’.
Fourth, it is interesting to consider the extent to which political factors, including affiliation of the proponent, are influential in the progress of Bills. The proponents of the seven Bills cover the political spectrum with the proponent of the (successful) Northern Territory Bill coming from the Country Liberal Party, two proponents from the Australian Labor Party, two from the Australian Democrats, two from the Australian Greens as well as an independent. However, this distribution is not proportionate to the affiliations of the proponents of the total number of Bills that were introduced. The percentage chance of a Bill being ‘close to passing’ is greater if the Bill is introduced by a member of a major political party, namely the Country Liberal Party or the Australian Labor Party. Of the 16 attempts by independents, only one was in the top seven Bills. Of the 19 attempts by a member of the Australian Greens, only two were in the top seven Bills. Furthermore, of the nine introduced by a member of the Australian Democrats, only two were in the top seven Bills. By contrast, of the six introduced by a member of the Australian Labor Party, two were in the top seven Bills; and the one Bill introduced by a member of the Country Liberal Party in the Northern Territory was successful.
What does not appear to be significant is the political persuasion of the government in power at the time the ‘close to passing’ Bills were debated. At the time the seven ‘close to passing’ Bills were introduced, the Country Liberal Party was in government in the Northern Territory, the Australian Labor Party was in government in Tasmania, and the Liberal Party was in power on two occasions and the Australian Labor Party was in power on three occasions when Bills were introduced in South Australia.
The final, and most remarkable, feature revealed by this analysis is that all of these seven Bills were introduced in the Northern Territory, South Australia and Tasmania, and five of the seven in South Australia. None of the 26 Bills introduced in the other jurisdictions satisfied the ‘close to passing’ criterion. Without further empirical research, it is difficult to know why this is the case. We can speculate that advocacy for controversial reform of this kind is more likely to succeed in smaller jurisdictions where there are fewer politicians who need to be persuaded for the Bill to succeed.[103]
However, there are likely to be a range of other issues at play as well. The high profile of either the proponent or supporter of the Bill has been a feature in each of the Northern Territory, South Australia and Tasmania Bills that have been ‘close to passing’. In the Northern Territory, Marshall Perron was the Chief Minister for much of the time that the reform Bill was being debated, but he was also seen as a passionate and charismatic advocate for change. The 2012 South Australian Bill that was narrowly defeated by two votes, although proposed by independent member Bob Such, was supported by the Premier, Jay Weatherill, as well as two senior ministers, Pat Conlon and Paul Caica.[104] In Tasmania, the proponents of the 2013 reform attempt were the Premier and leader of the Australian Labor Party, Larissa Giddings, as well as the leader of the Australian Greens, Nicholas McKim, both powerful political figures in that state.
Another feature that may be at play here, and identified by Plumb in her research of euthanasia reform activity in South Australia and Tasmania, is the power and influence of interest groups that support reform in those jurisdictions.[105] In South Australia, for example, there has been a long history of an active pro-euthanasia reform group. Plumb notes that the South Australian Voluntary Euthanasia Society (‘SAVES’), founded in 1983, has a large membership base and has consistently campaigned to reform the law.[106] She comments that a key strategy of SAVES is to increase visibility of the topic among politicians and the public, and refers to its monthly presence on the steps of Parliament where it distributes information pamphlets as well as displaying placards. An active pro-euthanasia lobby group, Dying with Dignity Tasmania, was also a feature in the Tasmanian 2013 campaign. In addition to running a public awareness campaign, Plumb notes that a key strategy of the group was to provide ‘good quality’ information to parliamentarians to assist them with their deliberations.[107]
The goal of Part III was to provide detail of reform attempts, the political context in which they occurred, and to make some observations about those reform attempts that came ‘close to passing’. In the next Part, we take a closer look at the Bills themselves.
Building on the above discussion of the general nature of the Bills introduced and whether they came ‘close to passing’, we will now analyse the critical features that have emerged from all the legislative models introduced into Australian parliaments. We will make specific reference to the seven Bills identified as being ‘close to passing’ to determine if there is anything significant in the legislative models adopted which may have impacted upon the ‘success’ of the Bill. Identifying the common elements of the legislative models – especially those that have been close to passing – is important because it may signal valuable information about what model might be close to achieving a consensus position in parliament. This information is useful for generating informed debate about reform in this context.
There are obviously many ways in which these legislative models can be classified and analysed. Some of these are substantive in that the law may permit different categories of behaviour, be it VE, PAS or both. Other modes of classification are structural in the sense that, if it does permit, say VE, PAS or both, there are different ways of doing so. For instance, it may provide that VE, PAS or both remain an offence, but create a defence to such conduct in certain circumstances. Alternatively, it may expressly decriminalise VE, PAS or both in certain specified circumstances. Finally, the legislative regimes can be grouped by examining procedural characteristics, including examining how eligibility is determined, for example in terms of illness and/or suffering criteria. This Part presents the analysis of the Australian legislative attempts in light of these various analytical approaches, but it should be borne in mind that there will be some overlap between them.
Perhaps the most fundamental substantive issue concerns whether the legislative models permit only VE, only PAS, or both. VE models permit the administration of a lethal substance by a physician to the patient. PAS models permit only the prescription of a lethal substance by medical practitioners – which the patient then administers to himself or herself. For some, this distinction is critical.[108]
Only one Australian Bill has been exclusively limited to VE. Subject to proposed safeguards, the Voluntary Euthanasia Bill 2010 (WA) provided that a medical practitioner may ‘administer euthanasia to the applicant by administration of a recognised drug’.[109] Clause 11(6) provided that it is unlawful for any person other than the patient’s medical practitioner to administer VE to the applicant. These provisions suggest that the legislation was limited to VE and was not intended to encompass PAS.[110] The reasons for this, and whether the omission was intentional, do not emerge from the limited debates surrounding the Bill.
The PAS model enables medical practitioners to allow patients, generally through the prescription of lethal substances, to terminate their own lives with, or without, the assistance of family members. The Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) is the only Australian Bill to permit solely PAS,[111] allowing a treating doctor to provide assistance to an ‘adult sufferer’ to terminate his or her life.[112]
All other Australian Bills allowed both VE and PAS. The ROTTIA is a prime example of this model. It provided that a patient who, in the course of a terminal illness, is experiencing pain, suffering and/or distress to an extent unacceptable to the patient, may request their doctor to assist them in terminating their life.[113] ‘Assist’ was defined to include the prescribing, preparation or giving of a substance to the patient for self-administration, and the administration of a substance to the patient.[114] By employing the phrase ‘the administration of
a substance’, the ROTTIA’s formulation of ‘assist’ exceeds mere PAS
and permits VE. This definition of ‘assist’ was also adopted, for example, in
New South Wales and Tasmanian Bills.[115] Another common approach uses the operative section, not the definitional provisions, to specify what constitutes administering VE.[116] For example, the Voluntary Euthanasia Bill 2002 (WA) expressly provided for the administration of a lethal substance to the patient by the medical practitioner, or the provision of substances for self-administration by the patient.[117]
Some South Australian Bills have widened their conception of VE. For example, the Voluntary Euthanasia Bill 2012 (SA) provided that a medical practitioner may administer VE to an adult suffering unbearable pain in the terminal phase of a terminal illness by (a) administering drugs in appropriate concentrations to end life; (b) prescribing drugs for self-administration by a patient to allow them to end their life; or (c) withdrawing or withholding medical treatment in circumstances which will result in an end to life.[118] The first ground contemplates VE; the second expands VE to incorporate PAS; while the third
ground incorporates the withholding or withdrawing of medical treatment which is legally[119] and, many would argue, conceptually or ethically distinct from VE.[120]
Legislative attempts to legalise VE can also be categorised as permissive, defence and penalty mitigation models. The permissive model provides a legislative framework, integrating appropriate safeguards, thereby positively allowing VE. This has been the most common model (35 Bills). We call it ‘permissive’ because, under such a model, if a medical practitioner complies with the requirements imposed under the framework, no offence is committed. The onus is on the prosecution to prove that the practitioner failed to comply with the provisions, beyond reasonable doubt. The defence model (2 Bills), by contrast, provides criteria which, if satisfied, will constitute an effective defence to a charge of murder or manslaughter. Under this model, VE and/or PAS would remain an offence, to which the defendant would have a defence if he or she can show, on the balance of probabilities, that he or she complied with the requirements of the defence provisions in the relevant Act. The penalty mitigation model substantially reduces associated penalties. These models will now be discussed.
The permissive model normally contains the following six critical elements:
1. power: power is conferred on treating medical practitioners to administer VE to certain eligible patients;[121]
2. immunity: immunity against civil, criminal or disciplinary liability is conferred on any persons assisting in the administration of VE in good faith;[122]
3. safeguards: protective procedures are generally prescribed to require competent requests, to provide information and to obtain psychiatric assessments; these and other safeguards are conditions precedent to exercising the relevant VE power or benefiting from the granted legal and disciplinary immunity (the safeguards are discussed further below);[123]
4. conscientious objections: a conscientious objections clause enables medical practitioners and institutions to decline to administer VE;[124]
5. avoidances: miscellaneous provisions to prevent contingency clauses in contracts, wills, insurance and annuities from adversely affecting the person’s entitlements on the basis of a request for VE;[125] and
6. oversight: various mechanisms are established for systematic oversight of the regime, for example a commission or committee that reviews deaths and/or reporting to parliament about how the legislation is being used.[126]
The ROTTIA once again illustrates the permissive model in use in Australia as it incorporates these six elements.[127]
As the permissive model actively permits the administration of VE or PAS, the safeguards employed require further discussion. The protective mechanisms in these Bills are generally directed towards ensuring the (1) accuracy of diagnosis and prognosis; (2) quality of the patient’s request including information requirements; and (3) voluntariness of the patient’s request. Quality of request refers to whether the patient has capacity and, even if he or she does, the quality of consideration that the patient has given to the decision. Voluntariness, by contrast, refers to whether the patient’s free will has been exercised to make the decision (in order for one’s will to be overborne or unduly influenced, one must at least have had the legal capacity to make the decision in the first place).
First, the most common legislative device applied to ensure the accuracy of the patient’s diagnosis and prognosis is requiring an independent physician to review the patient’s medical records, consult directly with the patient, and provide a second opinion. Variations of this requirement exist within all Australian Bills conforming to the permissive model.[128]
Second, information requirements, specialist consultations and cooling-off periods all ensure the quality of the patient’s decision. All Australian Bills make information requirements a condition of accessing VE or PAS and the medical practitioner’s personal immunity from prosecution or civil suit.[129] Information requirements enable patients to make a meaningful and autonomous decision
by informing them of the nature of their condition, its likely progress,
potential treatment options available, and the availability of supplementary support services.[130] Specialist consultations generally require the intervention of psychiatric or palliative care specialists. The principal function of the psychiatric evaluation is to ensure the patient is not adversely affected by a psychological condition affecting their capacity to make the request to receive VE or PAS. Psychiatric specialists ascertain whether the patient exhibits a treatable depressive or other psychiatric illness which may underpin the request for VE or PAS.[131] The psychiatric evaluation, therefore, operates as both an eligibility criterion and patient safeguard. The primary object of palliative care specialists is to ensure the patient is aware of palliative options to mitigate the physical, psychological and existential pain associated with their terminal illness.[132] The provision of cooling-off periods ensure the patient has the opportunity to understand information supplied by the medical practitioner and reconsider their decision. For example, the ROTTIA specified that the certificate of request could not be completed earlier than seven days from the initial request by the patient for their life to be terminated.[133]
Finally, in addition to issues that go to the capacity and quality of the decision, medical practitioners are also required to be satisfied on ‘reasonable grounds’ that the patient’s decision is voluntary and unaffected by duress or undue influence.[134] This is a separate issue from capacity, though it obviously overlaps with the issues discussed above concerning the quality of the actual decision made. We treat voluntariness separately, however, because it is normally a separately expressed requirement of its own in each of the models – whether the patient’s will has been overborne is in principle a different question from that of whether they have taken enough time to think about the decision or have made an adequately informed decision. Voluntariness is really about whether a decision in the true sense of the term has been taken by the patient at all. The requirement of ‘reasonable grounds’ imposes a positive duty on the practitioner to possess objective evidence that the request was voluntary. Supplementing the requirements of expert evaluation, most statutes regulating PAS and VE require a written request, generally within a prescribed form.[135] Writing requirements evidence both the request and that it originated from the patient rather than a third party.
As stated above, under a defence model, in strict terms, when the defence is made out, this means that the defendant has still committed an offence, but it is an offence for which he or she should not be held criminally responsible. Given this, why adopt such a model? A possible advantage of the defence model is that, by keeping VE or PAS prima facie an offence, the value of human life is considered to be protected, at least symbolically. The model represents the position that, while VE and PAS should not be actively permitted, medical practitioners subject to extraordinary demands, who elect to safely assist patients in terminating their life, should not be penalised. The disadvantage is that anyone who complies with the Act and so has a defence, has still committed an offence (it means that a doctor has effectively committed a murder or manslaughter) – it is just that the law considers it an offence for which the defendant should not
be criminally responsible. This disadvantage might explain why this model has
only been introduced sparingly within Australia – doctors or other medical practitioners probably do not want to consider themselves as committing offences for which the law will not hold them responsible and so this would make the defence model unpopular. When the defence model was introduced the one time in South Australia, it was seen as a legislative compromise designed to generate consensus regarding the legalisation of VE and PAS – that is, the advantage was privileged over the disadvantage. It was introduced as a way of attempting to respond to the failure of 16 permissive model Bills in that state.[136] Clause 3 of the Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) would have inserted a defence to a charge of a relevant offence under the Criminal Law Consolidation Act 1935 (SA). It would have been a defence to such a charge if the defendant could prove, on the balance of probabilities, that he or she acted in good faith in the ordinary course of the defendant’s employment, and that his or her conduct was a reasonable response to the patient’s suffering.[137]
There were other differences between the defence model in the South Australian Bill and the more standard permissive model. In contrast to the permissive models, the Bill merely required the request for VE or PAS to be ‘express’, as opposed to being reduced to writing or communicated within a prescribed form.[138] Furthermore, there was no requirement for expert consultation by psychiatric or palliative care specialists. The principal protective requirements were that the treating practitioner must be a qualified medical practitioner and the administration of VE or PAS must be a ‘reasonable response’ to the patient’s request.[139] Furthermore, unlike the permissive model, oversight and reporting mechanisms were notably absent. The details of whether the practitioner acted in good faith and whether the response in the circumstances was reasonable were to be left to the courts, which meant that parliament could avoid the danger of providing too many procedural requirements to be fulfilled before a practitioner could act on a patient’s request. This was a way of resolving the tension between the need to provide sufficient safeguards on the one hand, and the need to provide workable, practically orientated legislation, on the other.
The defence model adopted in the South Australian Bill contained the following elements:
• substantive defence: a person satisfying the relevant criteria incurs no civil, criminal or disciplinary liability;[140]
• exculpating criteria: these include requiring the relevant person to prove he or she was a treating practitioner;[141] that the person believed the adult to be of sound mind who was suffering from a medical condition which irreversibly rendered the patient’s quality of life intolerable;[142] that the patient expressly requested the VE;[143] and that the conduct was a reasonable response to the patient’s suffering;[144]
• accessorial liability: a defence was proposed, in certain circumstances, for any person who supported or assisted a medical practitioner in relation to the death of a person;[145]
• inchoate liability: the defences apply to circumstances where death was intended or suicide attempted, so it was not necessary to prove the patient in fact died;[146] and
• negativing fault elements: the defence could only be invoked if the conduct occurred in good faith without negligence.[147]
The penalty mitigation model was only introduced after the enactment of the Euthanasia Laws Act 1997 (Cth) which withdrew the legislative competence of the Australian territories to enact legislation permitting VE or PAS. There have been two such Bills. The relevant loophole the Bills attempted to exploit was that the Euthanasia Laws Act 1997 (Cth) deprived the territories of their power to enact legislation which permits, or has the effect of permitting, VE or PAS. The Bills, by imposing minor fines for committing VE according to prescribed procedural safeguards, arguably did not permit VE or PAS insofar as the practice remained prohibited, because it was still associated with criminal penalties. Clauses 3, 5 and 6 of the Crimes (Assisted Suicide) Bill 1997 (ACT) are examples.[148] The safeguards contained within the penalty mitigation model tend to be significantly less comprehensive than those in the permissive model. The above Australian Capital Territory Bill, for example, prescribed that requests for assistance must be in writing;[149] a cooling-off period of 72 hours;[150] and an independent medical practitioner must confirm that the patient was in a terminal phase of a terminal illness and suffering severe pain or distress.[151] While the imposition of writing requirements, cooling-off periods and limited independent consultation augments patient protection, the penalty mitigation model tends to lack the comprehensive protective frameworks contained within the permissive model.
It is also possible to categorise the models in terms of the nature of the illness that must be suffered by the person seeking assistance to die. Some Bills (which we call ‘exclusive’ models) only operated if the patient suffered from a terminal illness, or even the ‘terminal phase’ of a terminal illness.[152] There were 20 of these exclusive models. Other models (‘inclusive’ models) adopt a broader conception of the illnesses, including, for example, incurable and other chronic illnesses.[153] There were nine of these inclusive models. In one South Australian Bill, a defendant would have been entitled to a defence against criminal liability if the defendant could prove, among other things, that the person whose death resulted ‘from the administration of drugs ... by the defendant’ was suffering from a ‘qualifying illness’.[154] Under that Bill, a ‘qualifying illness’ meant ‘an illness, injury or other medical condition that irreversibly impaired the person’s quality of life so that life had become intolerable to that person’.[155] This provision would have allowed somebody who suffered an accident making them a quadriplegic to end their lives if they found life as a quadriplegic intolerable.
Pain and/or suffering[156] tends to be an essential eligibility criterion within most proposed Australian regulatory frameworks. Although some similarities exist between Bills, significantly different notions of the ‘pain’ and/or ‘suffering’ that must be endured before a person can be assisted to die are adopted. Distinctions lie in different conceptual requirements such as ‘existential suffering’, how pain and/or suffering is ascertained, and the causal connection between the illness and the relevant pain and/or suffering.[157]
There is an important distinction between pain and suffering. A person can ‘suffer’ if they experience pain, but need not experience pain in order to ‘suffer’. ‘Suffering’ is broader than pain and can include mental suffering and emotional suffering. In the case of the Bills introduced in Australia so far, the ‘nature’ of the pain and/or suffering required turns upon the label used to describe the ‘suffering’ and whether the terms appear together, either conjunctively or disjunctively, and on whether only one term is used or more than one is used. Many Bills and statutes refer to ‘pain’, ‘distress’ and ‘suffering’;[158] others to ‘pain’ and ‘distress’;[159] while others refer simply to ‘pain’.[160] The word ‘and’ means that the patient needs to be considered to be experiencing all or both, as the case may be. Likewise, if only one of the terms is used, especially the narrower term ‘pain’, this might (subject to a point we make in the next paragraph) limit the circumstances in which a request can be made. By contrast, where the word ‘or’ is used along with ‘pain’, ‘suffering’, and ‘distress’, the provisions are more expansive.
On the other hand, considering the substantial overlap between the concepts of ‘pain’, ‘distress’ and ‘suffering’, it is unclear to what extent the use of the single term ‘pain’ is distinguishable from the more expansive ones. For example, it is possible that ‘pain’ could be interpreted to encompass physical, mental and emotional suffering. Alternatively, a narrower understanding of the term might restrict it to physical pain. Whether the expanded or narrow definition is adopted would then depend on the relevant statutory framework.[161] If both ‘pain’ and ‘suffering’ are used in the same statute, then it is likely that ‘pain’ would be given the narrower reading – for it is a rule of statutory construction that all terms used in the statute be given a meaning, so the word ‘pain’ would arguably not be interpreted in such a wide way if the words ‘suffering’ (and ‘distress’) are also used. But of course any such restriction would be overcome by the use of the other terms that give it its restricted meaning in the first place.
A Victorian Bill provided that ‘intolerable suffering’ means ‘profound suffering and/or distress, whether physical, psychological or existential,
that is intolerable to the patient’.[162] Contrasting existential with physical and psychological suffering might suggest a different meaning of the term, incorporating, for example, a lack of ‘meaning’ within a person’s life, inability to self-actualise or severe despair. That said, even if this broader definition is adopted, ‘existential suffering’ possesses significant overlap with the concept of psychological suffering and, in practice, the two concepts may frequently be indistinguishable. The broadest concept of ‘suffering’ is contained within the Medical Treatment and Palliative Care (Voluntary Euthanasia) Amendment Bill 2008 (SA). It is defined to include the irreversible impairment of a person’s quality of life.[163] ‘Quality of life’ encompasses all relevant factors which may affect a person’s capacity for pleasure or displeasure.
The regulatory frameworks examined adopted diverse formulations of ‘pain’ and ‘suffering’, which are generally defined according to degree and durability. The degree of ‘pain’ and ‘suffering’ the patient must be experiencing varied between Bills and was defined using inexact phrases such as ‘severe’, ‘considerable’, ‘unbearable’ and ‘intolerable’. For example, the Rights of the Terminally Ill Bill 2001 (NSW) requires that a medical practitioner be satisfied the patient is experiencing ‘severe pain or suffering’ without defining the concept of ‘severe’.[164] The Voluntary Euthanasia Bill 2010 (WA) refers to a patient experiencing pain, suffering or debilitation which is ‘considerable’.[165] Other Bills refer to pain the person finds ‘unbearable’,[166] and so is defined by reference to the individual’s subjective experience.[167] ‘Intolerable suffering’ is another phrase used which, again, is defined subjectively as profound suffering or distress which is intolerable to the patient.[168]
The distinction between ‘considerable’, ‘unbearable’, ‘severe’ and ‘intolerable’ pain and/or suffering is a question of degree. A patient experiencing ‘considerable’ pain may not be in ‘severe’ pain and may not be experiencing ‘unbearable’ or ‘intolerable’ pain. ‘Intolerable’ or ‘unbearable’, by contrast,
seem to be synonymous. The difference in degree only becomes relevant
as a procedural criterion where there is an objective arbiter. The Rights of
the Terminally Ill Bill 2001 (NSW) implicitly suggests that the question
as to whether the patient is suffering ‘severe’ pain will be a matter of
medical judgment.[169] However, contemporary medical practice recognises that the capacity of a person to withstand pain varies between individuals.[170] More commonly, however, Bills such as the Dying with Dignity Bill 2009 (Tas) and Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) require the patient to make the assessment, stating that the pain must be unacceptable to the patient.[171] When the patient is the arbiter of the pain, the semantic distinction between differing degrees of suffering dissolves. Some Bills, such as the Voluntary Euthanasia Bill 2010 (WA), are silent in relation to the arbiter of the degree of pain the patient suffers.[172]
The ‘durability’ of pain or suffering, or both pain and suffering, must be distinguished from the irreversibility or incurability of the illness. An illness
may be irreversible or incurable, but painless, though presumably one can
‘suffer from’ an irreversible or incurable illness. Here, though, ‘suffer’ just means to have or experience the illness and must be distinguished from the kind
of suffering that accompanies the illness or medical condition, which the use of the word ‘suffering’ is intended to refer to. Durability may be defined as continuous or long-lasting pain or suffering. The requirement of ‘durability’ or repeated requests is also contemplated within statutes with cooling-off periods.[173] Incorporated within the concept of durability is pain mitigation. This question is distinct from curability because it relates to pain palliation or, if the symptoms do not cause pain, suffering palliation. The ROTTIA, for example, imposes a requirement that palliative care must be unable to alleviate pain and/or suffering to levels acceptable to the patient.[174]
The various Bills also differ in terms of the required nexus between suffering and/or pain on the one hand, and illness on the other. Some Bills expressly require an objective causal relationship between the illness and the suffering.[175] For example, under the Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic), the treating doctor must be reasonably satisfied that the sufferer has a terminal or incurable illness that is causing the patient intolerable suffering.[176] Other Bills merely require the existence of a ‘relationship’ between illness and the pain and/or suffering. For example, the Voluntary Euthanasia Bill 2010 (WA) requires the patient to experience pain, suffering or debilitation that is ‘related to the relevant terminal illness’.[177]
The concept of ‘causation’ would clearly encompass pain and/or suffering directly deriving from the illness as a causative factor, but, on a broad interpretation, may also incorporate the existential pain a professional athlete may experience on discovering that, by reason of some debilitating illness or disability, they may never compete again. In contrast, and depending on the conception of causality adopted, it would not encompass a request for VE pursuant to significant existential pain deriving from, say, a partner divorcing the patient after he or she contracts the terminal illness.
However, this existential pain may fall within the ambit of the Voluntary Euthanasia Bill 2010 (WA) because there is a relationship between the divorce and the terminal illness, even where the terminal illness was merely connected, and not necessarily a determinative or significantly contributing factor, to the divorce. There may be other examples, such as where a pre-existing psychological illness is exacerbated, but not necessarily caused, by a terminal illness, and the psychiatric disorder is the primary motivation underpinning the request for VE. In jurisdictions adopting a causal criterion, the court is likely to adopt either the ‘but for’ or ‘material contribution’ tests for causation.[178] Where the ‘but for’ test is adopted, the distinction between requiring a causal relationship rather than a mere relationship becomes more evident. However, if the court adopts the material contribution test, the judiciary may determine that a causal relationship exists notwithstanding that existential, psychological or physical pain derives from a combination of the terminal illness and other related sources. Regardless of which test is selected, in the majority of cases, it is unlikely that the distinction between the requirement for causality and a mere relationship will be determinative.
The majority of VE Bills adopt a current request model (21 in total), which allows a person to make a request for assistance to die only while he or she has capacity.[179] By contrast, an advance request model (of which there have been eight), where a request continues to operate if the person subsequently loses legal capacity, has been adopted by the South Australian Dignity in Dying Bills introduced in 2001–05, which provide for an advance request to be made by a person who is not yet ‘hopelessly ill’.[180] Finally, some VE Bills have permitted surrogate decision-making.[181]
Most legislative models provide for oversight of VE and PAS practice. There are two common oversight mechanisms: (a) establishing a monitoring and reporting entity; or (b) utilising an existing entity for monitoring and reporting purposes. In Australia, the vast majority of Bills permitting VE or PAS opt for the second approach and require medical reporting to the coroner, who is responsible for monitoring, evaluating and reporting on the operation of the system.[182]
The models introduced in Australia exhibit many similarities. The overwhelming majority of proposed frameworks adopt the permissive model –
35 of the 39 Bills, including all of those that were ‘close to passing’.[183] In all Australian Bills (and the repealed Northern Territory Act), assistance to die would be available only to an adult who is enduring pain or suffering and/or has a terminal illness. The person is to be competent at the time of the request, and the request must be made voluntarily – that is, even when made by a person who has capacity, it is not made under duress or undue influence. Under some models, assistance to die can be given to a person who no longer has capacity provided the request was made when he or she did have capacity.[184] Rarely, the legislative proposal allows the request to be made under a power of attorney.[185] Generally, the individual was permitted to determine whether his or her suffering satisfied the required pain threshold to receive VE or PAS.[186] Most Australian Bills adopted a broad interpretation of the categories of pain and suffering, frequently including physical, psychological and existential pain.[187]
Most Australian Bills contain consultative requirements which may necessitate obtaining information from independent medical, psychiatric or palliative care specialists.[188] These consultative requirements facilitate specialist assessment about whether the individual is suffering a treatable psychiatric condition, which could vitiate a request for VE or PAS,[189] or acting under duress or undue influence.[190] Most Bills require written requests using a prescribed form,[191] and incorporate cooling-off periods.[192] A number of Bills incorporate residency requirements restricting the availability of VE,[193] although this was not a feature of the Northern Territory legislation. As an oversight measure, the vast majority of Bills permitting VE or PAS require medical reporting to the coroner, who is responsible for monitoring, evaluating and reporting on the system.[194]
In Part III above, we stated that seven of the Bills introduced into Australia were ‘close to passing’ (as we have defined that term). Are there any features of these Bills, when compared to those that did not meet this threshold, which might explain why they were able to get so far? For instance, did the provisions concerning safeguards in these Bills have anything in common that would suggest that members of parliament were close to believing that the provisions addressed well-known concerns about these safeguards? Or did the Bills only make lawful VE or PAS in circumstances where a person is terminally ill, thereby limiting the range of circumstances in which a person can avail themselves of the new laws and so making the Bill more palatable for the members of parliament who had to vote on it? Again, were the Bills that were close to passing restricted to PAS, VE, or did they include both? There are certainly common features in these Bills, but none of these features sets them apart from the features of many of the other Bills we have mentioned that were not close to passing. And there were also differences among the Bills on the issues that normally remain controversial, such as whether the Bills were restricted to terminal illnesses only, and whether they regulated only PAS or only VE, or included both. Two of the South Australia Bills that were close to passing, for instance, were not limited to terminal illness.[195] This seems to speak against the idea that a Bill has a greater chance of passing if it is restricted to cases where a patient is terminally ill.[196] Finally, all the Bills that came close to passing contemplated both PAS and VE. There was no restriction exclusively to one or the other, as one might have expected if a more restricted proposal were put forward. There is no sound basis for concluding that the nature of these Bills made them go further than the nature of the Bills that did not come close to passing.
This article has examined two decades of attempted VE reform in Australia. The trends over this period were explored, along with the extent to which Bills progressed (or did not progress) through the relevant houses of parliament. The analysis of reform attempts was also considered in a political context and some tentative conclusions were drawn about why some Bills gained more political support than others. The second half of the article focused on analysing the various models that have been advanced to change the law, including examining them through different lenses (substantive, structural and procedural). This analysis concluded by determining typical approaches to proposed reform in Australia, namely a permissive model that covers both VE and PAS and is limited to competent adults who are terminally or incurably ill and experiencing suffering (variously defined). Multiple safeguards are proposed and there are official oversight mechanisms, generally involving reporting to the coroner.
The authors predict that VE law reform is likely to occur in Australia. There is a convergence of factors that make this issue increasingly difficult for politicians to ignore: high and sustained public support for reform in Australia; an ageing and increasingly informed population seeking choices for their end-of-life experience; the changing legal landscape internationally; and the media’s interest in the topic and, particularly for social media, its agitation for change. These factors are evidenced by an increasing trend of parliamentary activity in this area such as through the introduction of Bills, the release of exposure drafts of Bills and the establishment of select committees. And once the first state or territory enacts legislation, others are likely to follow.
As to when that occurs, no doubt the prevailing political context will be critical. And, in that regard, we make two concluding observations. The first is that who the proponent for reform is may be decisive in whether or not it succeeds. Marshall Perron was the proponent of the only VE Bill ever to have succeeded in Australia, and he was (for much of the relevant time at least) the Chief Minister in the Northern Territory as well as being seen as a popular and charismatic character. Two of the other Bills that we classified as ‘close to passing’ were supported by high-profile politicians including Larissa Giddings and Nicholas McKim (the 2013 Bill in Tasmania) and Jay Weatherill, Pat Conlon and Paul Caica (the 2012 Bill in South Australia). This observation, if correct, has implications for the immediate future now that Richard Di Natale, who has released an exposure draft of a Bill advocating for reform, is leader of the Australian Greens. The second point is that we can be confident that politicians will engage with the issue of VE reform more directly if the public places it on the political agenda, as opposed to merely supporting the concept of reform when their views are sought in opinion polls. Given the increasing extent to which euthanasia reform is becoming part of the political discourse in the lead up to elections, it may be that we are approaching the point where major political parties may be forced to develop policy positions on reform.
Given reform efforts to date, the model described above is likely to be the one enacted in Australia. But despite a broadly consistent approach taken nationally, there are still important legislative choices to be made. For example, the word ‘suffering’ can encompass different aspects of a person’s experience and can also be judged from different perspectives. The analysis undertaken in this article can be of assistance for legislators and policymakers in identifying and unpacking choices such as these. While the international experience is outside the scope of this article, some of the features of the Australian models are consistent with international models. This points to the need to learn from the experiences of those jurisdictions. There is now an increasing body of empirical evidence as to the operation of these VE and/or PAS regimes and this needs to be considered when deciding whether to undertake reform or not, and the actual design of proposed reforms.[197]
The enactment of legislation that provides state imprimatur for a health professional (or another) to end a person’s life (or provide assistance for a person to take their own life) is a significant step, and should be recognised as such. Concerns about the effect of such a shift on the community and particularly the vulnerable within our community have been an important part of the debate for many decades. It is not the purpose of this article to engage with the merit or otherwise of these arguments but one of the key considerations when proposing law reform is to consider carefully how and if a model for VE and/or PAS addresses these issues. To assist with those deliberations, we offer the analysis in this article of the various Bills that have been introduced into Australian parliaments to date. The authors hope that this analysis will inform community debate, too frequently littered with inaccurate claims about what is or has been proposed when VE or PAS Bills are drafted. We also hope that this article will assist in cultivating a more sophisticated understanding of the various regulatory models, and the options that are available to parliaments when considering legislative reform.
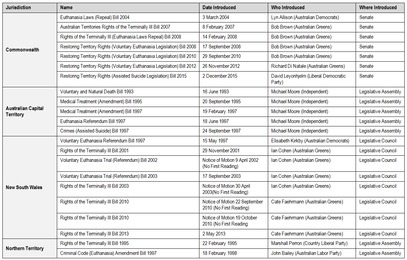
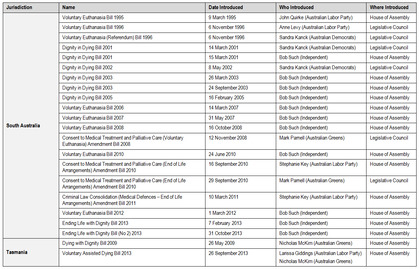

[*] BCom (UQ), LLB (Hons) (UQ), LLM (Cantab), PhD (QUT), Professor, Australian Centre for Health Law Research, Faculty of Law, Queensland University of Technology.
[**] LLB (Hons) (QUT), DPhil (Oxf), Professor, Australian Centre for Health Law Research, Faculty of Law, Queensland University of Technology.
[***] LLB/BBus, Faculty of Law, Queensland University of Technology.
[****] BA/LLB (Hons) (UNE), PhD (UNE), Senior Lecturer, Australian Centre for Health Law Research, Faculty of Law, Queensland University of Technology.
[*****] BA (Hons) (Lancaster), LLB (Hons) (QUT), LLM (QUT), PhD (Essex), Senior Lecturer, Australian Centre for Health Law Research, Faculty of Law, Queensland University of Technology.
The authors wish to thank Stephanie Jowett for her research assistance. This article is an accurate statement of the law as at 31 December 2015.
[1] Ending Life with Dignity Bill 2013 (SA); Rights of the Terminally Ill Bill 2013 (NSW); Voluntary Assisted Dying Bill 2013 (Tas).
[2] Larissa Giddings and Nicholas McKim, Voluntary Assisted Dying: A Proposal for Tasmania (Consultation Paper, February 2013) <http://stors.tas.gov.au/941696> Gareth Griffith and Lenny Roth, ‘Euthanasia’ (Issues Backgrounder, Parliamentary Library, Parliament of New South Wales, 2013) <http://www.parliament.nsw.gov.au/prod/parlment/publications.nsf/key/Euthanasia/$File/Euthanasia+Issues+Backgrounder+update.pdf> . See also a report released by the independent think tank, Australia21, calling for reform in this area: Bob Douglas, Lindy Willmott and Ben White, ‘The Right To Choose an Assisted Death: Time for Legislation?’ (Report, Australia21, April 2013) <http://www.australia21.org.au/
wp-content/uploads/2013/08/J2056-Assisted-Death-Report_WEB.pdf>. This report followed an Australia21 round table hosted by the Australian Centre for Health Law Research at the Queensland University of Technology in January 2013, which was informed by a background paper produced for the event. The background paper was later published as: Ben White and Lindy Willmott, ‘How Should Australia Regulate Voluntary Euthanasia and Assisted Suicide?’ (2012) 20 Journal of Law and Medicine 410.
[3] Senate, Parliament of Australia, Medical Services (Dying with Dignity) Exposure Draft Bill 2014 (2014) <http://www.aph.gov.au/~/media/Committees/Senate/committee/legcon_ctte/dying_with_dignity/
Exposure%20draft%20dying%20with%20dignity.pdf>.
[4] Restoring Territory Rights (Assisted Suicide Legislation) Bill 2015.
[5] See, eg, Australian Greens, Greens To Take ‘Dying with Dignity’ to Canberra (15 August 2013) <http://greens.org.au/greens-take-%E2%80%98dying-dignity%E2%80%99-canberra> Voluntary Euthanasia Party, Party Policy (2015) <http://www.vep.org.au/policy> Australian Sex Party, Federal Euthanasia Policy (2015) <http://www.sexparty.org.au/policy/3-federal-euthanasia-policy> .
[6] See, eg, Australian Broadcasting Corporation, ‘Australia’s First Euthanasia Clinic Opens’, 7.30 Report, 5 December 2013 (Alex Mann) <http://www.abc.net.au/7.30/content/2013/s3906089.htm> Megan Doherty, ‘Euthanasia: Time To Talk’, The Canberra Times (Canberra), 27 July 2013, 1; Daniel Wills, ‘New Euthanasia Bid Fails’, The Advertiser (Adelaide), 15 June 2012, 5; Matthew Denholm, ‘Premier Sponsors State Euthanasia Bill’, The Australian (Sydney), 27 September 2013, 6; George Williams, ‘Tasmania Leads Way on Voluntary Euthanasia’, Sydney Morning Herald (Sydney), 27 February 2013, 9; Australian Broadcasting Corporation, ‘Euthanasia Campaigner under Scrutiny’, 7.30 Report, 18 December 2012 (Mike Sexton) <http://www.abc.net.au/7.30/content/2012/s3657550.htm> Bruce Mounster, ‘Nitschke Visit Stirs Euthanasia Debate’, The Mercury (Hobart), 17 February 2012, 13; Graham Watson, ‘Euthanasia Sense’, Saturday Extra, The Northern Territory News (Darwin), 23 March 2013, 21; David Harradine, ‘Economy of Euthanasia Woes’, The Mercury (Hobart), 9 October 2013, 22; Aryelle Sargent, ‘McKim Euthanasia Case’, Advocate (Burnie, Tasmania), 11 October 2013, 3; Matt Smith, ‘Euthanasia Bill Reborn’, The Mercury (Hobart), 4 February 2013, 5.
[7] See, eg, Carter v A-G (Qld) [2013] QCA 140; [2014] 1 Qd R 111; R v Klinkerman [2013] VSC 65; R v Nielsen [2012] QSC 29; R v Justins [2011] NSWSC 568; R v Maxwell [2003] VSC 278; DPP (Vic) v Karaca [2007] VSC 190; R v Nicol [2005] NSWSC 547; DPP (Vic) v Nestorowycz [2008] VSC 385; DPP (Vic) v Rolfe [2008] VSC 528; (2008) 191 A Crim R 213; R v Hood [2002] VSC 123; (2002) 130 A Crim R 473.
[8] Wet toetsing levensbeëindiging op verzoek en hulp bij zelfdoding 2000 [Termination of Life on Request and Assisted Suicide Act 2000] (Netherlands).
[9] Loi relative à l’euthanasie 2002 [Act on Euthanasia 2002] (Belgium).
[10] Loi du 16 mars 2009 sur l’euthanasie et l’assistance au suicide [Law of 16 March 2009 on Euthanasia and Assisted Suicide] (Luxembourg) JO, 16 March 2009, 615.
[11] Death with Dignity Act, Or Rev Stat §§ 127.800–127.995 (1994).
[12] Death with Dignity Act, Wash Rev Code §§ 70.245.010–70.245.904 (2008).
[13] Patient Choice and Control at End of Life Act, Vt Stat Ann §§ 5281–93 (2013).
[14] End of Life Option Act, Cal Health and Safety Code §§ 443–443.22 (2015).
[15] Act Respecting End-of-Life Care, RSQ 2014, c S-32.0001.
[16] The Strafgesetzbuch [Criminal Code] (Switzerland) was not specifically amended (ie, after its enactment) to permit assisted suicide for unselfish reasons. In the first draft of the Bill in 1893 prepared by its progenitor, Carl Stooss, the draft code prohibited assisted suicide for all reasons. However, a criminal law professor, Ernst Hafter, before the adoption of the draft code, argued that only where a person provides assistance to suicide for selfish motives should they be exposed to criminal penalties. Hafter’s arguments stimulated debate, and were taken into account by the draft code prepared by the Federal Council in 1918 under the then art 102. The debate surrounding the inclusion of the selfish motives clause within the draft code, surprisingly, did not entail any material discussion of medically assisted dying (unlike the present art 114), but rather focused on the philosophical complexities of criminalising the assistance of a non-criminal act, and romantic notions appertaining to ‘honour’ suicides, or the suicide of rejected lovers. The draft code was adopted by referendum in 1938, which included the amended provisions, and entered into force in 1942. Therefore, the ‘selfish reasons’ element has always been present in Swiss law since the codification of the criminal law: Olivier Guillod and Aline Schmidt, ‘Assisted Suicide under Swiss Law’ (2005) 12 European Journal of Health Law 25; National Advisory Commission on Biomedical Ethics, Assisted Suicide (Opinion No 9/2005, 27 April 2005) 31 <http://www.nek-cne.ch/fileadmin/nek-cne-dateien/Themen/Stellungnahmen/en/suizidbeihilfe_en.pdf> .
[17] Carter v A-G (Canada) [2015] 1 SCR 331.
[18] Criminal Justice Branch, Ministry of Attorney General (British Columbia), Euthanasia and Assisted Suicide (Crown Counsel Policy Manual No 56880-00, 15 March 2004) <http://www.ag.gov.bc.ca/
prosecution-service/policy-man/pdf/EUT1-EuthanasiaAndAssistedSuicide-15Mar2004.pdf>. For a critique of these guidelines, see Jocelyn Downie and Ben White, ‘Prosecutorial Discretion in Assisted Dying in Canada: A Proposal for Charging Guidelines’ (2012) 6(2) McGill Journal of Law and Health 113.
[19] In R (Pretty) v DPP (UK) [2001] UKHL 67; [2002] 1 AC 800 and Pretty v United Kingdom [2002] III Eur Court HR 427, the House of Lords and the European Court of Human Rights rejected the existence of a right to PAS or VE. However, in R (Purdy) v DPP (UK) [2009] UKHL 45; [2010] 1 AC 345, the House of Lords concluded that, pursuant to arts 8(1)–(2) of the Convention for the Protection of Human Rights and Fundamental Freedoms, opened for signature 4 November 1950, 213 UNTS 222 (entered into force 3 September 1953), as amended by Protocol No 14bis to the Convention for the Protection of Human Rights and Fundamental Freedoms, opened for signature 27 May 2009, CETS No 204 (entered into force 1 September 2009) (‘European Convention on Human Rights’), the code for Crown Prosecutors was required to provide greater guidance to promote accessibility and foreseeability in prosecutions, and therefore a more specific policy identifying the facts and circumstances relevant to the institution of criminal proceedings should be established. For the prosecutorial guidelines, see Director of Public Prosecutions (UK), Policy for Prosecutors in Respect of Cases of Encouraging or Assisting Suicide (February 2010) Crown Prosecutor Service <http://www.cps.gov.uk/publications/prosecution/assisted_suicide_policy.html> . For commentary on these guidelines, see Ben White and Jocelyn Downie, ‘Prosecutorial Guidelines for Voluntary Euthanasia and Assisted Suicide: Autonomy, Public Confidence and High Quality Decision-Making’ (2012) Melbourne University Law Review 656; Penney Lewis, ‘Informal Legal Change on Assisted Suicide: The Policy for Prosecutors’ (2011) 31 Legal Studies 119; Glenys Williams, ‘Assisting Suicide, the Code for Crown Prosecutors and the DPP’s Discretion’ (2010) 39 Common Law World Review 181; Alexandra Mullock, ‘Overlooking the Criminally Compassionate: What Are the Implications of Prosecutorial Policy on Encouraging or Assisting Suicide?’ (2010) 18 Medical Law Review 442.
[20] That is, when the Voluntary and Natural Death Bill 1993 (ACT) was presented: ACT Government, Voluntary and Natural Death Bill 1993 (Discharged), ACT Legislation Register <http://www.legislation.
act.gov.au/b/db_15844>.
[21] Within this figure of 51, the authors have included the attempts at a Commonwealth level to abolish the Euthanasia Laws Act 1997 (Cth) which deprives the territories of the power to pass legislation legalising VE or PAS.
[22] In 1962, the earliest Morgan Gallup poll indicated VE support was at 47 per cent. Similar polls were conducted on a regular basis until 1995 when public support for VE had increased to 78 per cent: Margaret F A Otlowski, Voluntary Euthanasia and the Common Law (Clarendon Press, 1997) 263. More recent polls from varying sources (Morgan Poll, Newspoll and other independently administered surveys) in 2002–12 indicate that national support has varied between 78 per cent and 85 per cent: Your Last Right, Australian Public Desire for Legalisation of Assisted Dying in Restricted Circumstances (White Paper, 2012) <http://www.dwdnsw.org.au/documents/2013/POLL%20WHITE%20PAPER%
202012.pdf>; South Australian Voluntary Euthanasia Society, Public Opinion Polls on Voluntary Euthanasia Law Reform in Australia (Factsheet No 02, 2012) <http://www.saves.asn.au/facts/fs02.pdf> .
[23] See, eg, Dan Harrison, ‘MPs from Both Sides Back Euthanasia Reform’, Sydney Morning Herald (online), 11 November 2014 <http://www.smh.com.au/federal-politics/political-news/mps-from-both-sides-back-euthanasia-reform-20141111-11kis9.html> Staff Writers, ‘Let’s Settle This: Should Australia Legalise Euthanasia?’, The Courier Mail (online), 4 September 2014 <http://www.couriermail.com.au/
news/lets-settle-this-should-australia-legalise-euthanasia/story-fnihsrk2-1227047380264>; Bob Douglas, ‘The Right to Assisted Death’, Comment, The Canberra Times (online), 20 May 2013 <http://www.canberratimes.com.au/comment/the-right-to-assisted-death-20130519-2juwp.html> Josephine Tovey, ‘Euthanasia Is Just a Bridge Too Far’, Sydney Morning Herald (Sydney), 23 October 2012, 1.
[24] See, eg, White and Willmott, above n 2; Lorana Bartels and Margaret Otlowski, ‘A Right To Die? Euthanasia and the Law in Australia’ (2010) 17 Journal of Law and Medicine 532; Brian Pollard, ‘Fatal Licence: Commentary on the “Consent to Medical Treatment and Palliative Care (Voluntary Euthanasia) Amendment Bill 2008”’ (2010) 22(2) Bioethics Research Notes 19; Bob Brown, ‘The Right To Die: Legislating for Euthanasia’ (2008) 89 Precedent 29; Alan Rothschild, ‘Physician-Assisted Death: An Australian Perspective’ in Dieter Birnbacher and Edgar Dahl (eds), Giving Death a Helping Hand – Physician-Assisted Suicide and Public Policy: An International Perspective (Springer-Verlag, 2008).
[25] This table is based on that included in White and Willmott, above n 2, 412.
[28] Australian Capital Territory, Parliamentary Debates, Legislative Assembly, 16 June 1993, 1878–9 (Michael Moore).
[29] See Voluntary and Natural Death Bill 1993 (ACT) long title, cl 4.
[30] See Voluntary and Natural Death Bill 1993 (ACT) long title, cl 21. This aspect of the proposed Bill clarified the common law position that withholding and withdrawing treatment was lawful in some circumstances.
[31] Voluntary and Natural Death Bill 1993 (ACT) cls 4–6.
[32] Australian Capital Territory, Parliamentary Debates, Legislative Assembly, 14 April 1994, 818 (Michael Moore).
[33] Select Committee on Euthanasia, Parliament of the Australian Capital Territory, Report: Voluntary and Natural Death Bill 1993 (1994) 6–7.
[34] Ibid.
[35] Australian Capital Territory, Parliamentary Debates, Legislative Assembly, 11 May 1994, 1377 (Michael Moore).
[36] Despite the Voluntary and Natural Death Bill 1993 (ACT) being discharged, Parliament enacted the Medical Treatment Act 1994 (ACT) which was limited to the withholding and withdrawal of medical treatment, and the making of directions and powers of attorney in relation to withholding and withdrawal of treatment that would apply after the patient has lost capacity.
[37] Medical Treatment (Amendment) Bill 1995 (ACT); Medical Treatment (Amendment) Bill 1997 (ACT); Euthanasia Referendum Bill 1997 (ACT); Crimes (Assisted Suicide) Bill 1997 (ACT).
[38] Interestingly, Marshall Perron is the only member affiliated with the Liberal Party (he was the leader of the Country Liberal Party in the Northern Territory) to have introduced a Bill pertaining to VE.
[39] Northern Territory, Parliamentary Debates, Legislative Assembly, 22 February 1995, 2495 (Marshall Perron).
[40] Ibid 2505–28 (Shane Stone).
[41] Select Committee on Euthanasia, Parliament of the Northern Territory, The Right of the Individual or the Common Good? Report of the Inquiry by the Select Committee on Euthanasia (1995) 64–6.
[42] Northern Territory, Parliamentary Debates, Legislative Assembly, 24 May 1995, 3734.
[43] Ibid 3782.
[44] Northern Territory (Self-Government) Act 1978 (Cth); Australian Capital Territory (Self-Government) Act 1988 (Cth); Norfolk Island Act 1979 (Cth).
[45] Commonwealth, Parliamentary Debates, House of Representatives, 9 September 1996, 3672 (Kevin Andrews).
[46] Commonwealth, Parliamentary Debates, House of Representatives, 9 December 1996, 8060 (Robert Halverson, Speaker).
[47] Ibid 8078 (Robert Halverson, Speaker).
[48] Commonwealth, Parliamentary Debates, Senate, 12 December 1996, 7358–60 (John Herron).
[49] Commonwealth, Parliamentary Debates, Senate, 24 March 1997, 2326 (Margaret Reid).
[50] Ibid 2331 (Margaret Reid).
[51] Euthanasia Laws Act 1997 (Cth) s 2.
[52] Euthanasia Laws (Repeal) Bill 2004 (Cth), introduced by Lyn Allison: Commonwealth, Parliamentary Debates, Senate, 3 March 2004, 20 717 (Lyn Allison).
[53] These Bills have been:
• Australian Territories Rights of the Terminally Ill Bill 2007 (Cth), introduced by Bob Brown: Commonwealth, Parliamentary Debates, Senate, 8 February 2007, 17 (Bob Brown);
• Rights of the Terminally Ill (Euthanasia Laws Repeal) Bill 2008 (Cth), introduced by Bob Brown: Commonwealth, Parliamentary Debates, Senate, 14 February 2008, 335 (Bob Brown);
• Restoring Territory Rights (Voluntary Euthanasia Legislation) Bill 2008 (Cth), introduced by Bob Brown: Commonwealth, Parliamentary Debates, Senate, 17 September 2008, 4983 (Bob Brown);
• Restoring Territory Rights (Voluntary Euthanasia Legislation) Bill 2010 (Cth), introduced by Bob Brown: Commonwealth, Parliamentary Debates, Senate, 29 September 2010, 304 (Bob Brown); and
• Restoring Territory Rights (Voluntary Euthanasia Legislation) Bill 2012 (Cth), introduced by Richard Di Natale: Commonwealth, Parliamentary Debates, Senate, 26 November 2012, 9737 (Richard Di Natale).
[54] Restoring Territory Rights (Assisted Suicide Legislation) Bill 2015. This Bill is still before the Senate.
[55] A trendline is a simplified line of best fit demonstrating the direction of a correlation between a dependent and independent variable.
[56] Between 1993 and 1997, 11 Bills were introduced into Australian parliaments. Seven were introduced in the Northern Territory and the Australian Capital Territory. The remaining four were introduced in the other six jurisdictions over this time period, making an average of only 0.67 Bills per jurisdiction.
[57] This calculation is taken from 1998 to 2015.
[58] The average number of Bills introduced into Australian parliaments between 2007 and 2013 was 3.29 annually. In 2014 and 2015, only one VE Bill was introduced.
[59] But see Alison Plumb, ‘The Future of Euthanasia Politics in the Australian State Parliaments’ (2014) 29 Australasian Parliamentary Review 67, which considered the role of politics and political affiliation in this context in SA and Tasmania.
[60] Australian Greens, Dying with Dignity <http://greens.org.au/dying-with-dignity> .
[61] The Australian Democrats 2010 Action Plans expressly supported the enactment of nationally consistent VE laws: Australian Democrats, Australian Democrats Action Plans 2010 <http://australian-democrats.org.au/action-plans-2010.php#.VmJW4GDotMs> . This reference was removed from its 2013 Action Plans: Australian Democrats, Australian Democrats Action Plans <http://australian-democrats.org.au/policies2013.php#.VmJW7mDotMs> .
[62] Note that this includes the Voluntary Assisted Dying Bill 2013 (Tas), which was a joint initiative of the Australian Greens and the Australian Labor Party.
[63] Note that this includes the Voluntary Assisted Dying Bill 2013 (Tas), which was a joint initiative of the Australian Greens and the Australian Labor Party.
[64] Note, however, this is not always the case, as noted by Plumb, above n 59 in the context of two attempts to reform in SA and Tasmania.
[65] Australian Capital Territory, Parliamentary Debates, Legislative Assembly, 5 November 1997, 3672 (Michael Moore).
[66] Ibid 3673 (Michael Moore).
[67] New South Wales, Parliamentary Debates, Legislative Council, 13 November 2003, 4931 (Ian Cohen).
[68] New South Wales, Parliamentary Debates, Legislative Council, 15 May 1997, 8659 (Elisabeth Kirkby).
[69] Tasmania, Parliamentary Debates, House of Assembly, 17 October 2013, 114 (Tim Morris); New South Wales, Parliamentary Debates, Legislative Council, 23 May 2013, 20 785 (Don Harwin).
[70] This practice has resulted in allegations of political gamesmanship: New South Wales, Parliamentary Debates, Legislative Council, 23 May 2013, 20 781 (Cate Faehrmann); Tasmania, Parliamentary Debates, House of Assembly, 16 October 2013, 118 (Michelle O’Byrne).
[71] Cf the views expressed by Neil Francis, a pro-euthanasia advocate and Chief Executive Officer of YourLastRights.com Ltd in Neil Francis, ‘Australian Public Desire for Legislation of Assisted Dying in Restricted Circumstances’ (White Paper, YourLastRight.com, 2012). The white paper is based on research undertaken by Newspoll and commissioned by YourLastRights.com Ltd. In that white paper, it is suggested that ‘[m]ore than a quarter of all voters (29%) will change their vote if their otherwise most likely candidate or party’s stance on assisted dying law reform is opposed to their own stance’ and that ‘[a] politician whose stance is opposed to assisted dying law reform will lose significantly more votes at a general election (23%) than a politician who supports reform (6%)’: at [1] (emphasis altered).
[72] Christoffer Green-Pedersen, ‘The Conflict of Conflicts in Comparative Perspective: Euthanasia as a Political Issue in Denmark, Belgium, and the Netherlands’ (2007) 39 Comparative Politics 273.
[73] See, eg, Brenton Prosser and Richard Denniss, Minority Policy: Rethinking Governance When Parliament Matters (Melbourne University Press, 2015). See also media commentary on the rise in political influence of minor parties: Ross Fitzgerald, ‘The Major Threat of Minor Parties in New Senate’, The Australian (online), 7 June 2014 <http://www.theaustralian.com.au/opinion/columnists/the-major-threat-of-minor-parties-in-new-senate/story-e6frg7eo-1226946409257> Antony Green, ‘Record Vote for Minor Parties at 2013 Federal Election’ on Antony Green, ABC Elections: Antony Green’s Election Blog (19 November 2013) <http://blogs.abc.net.au/antonygreen/2013/11/record-vote-for-minor-parties-at-2013-federal-election.html> .
[74] See, eg, The Australian & New Zealand Society for Palliative Medicine Inc, The Practice of Euthanasia and Assisted Suicide (Position Statement, 31 October 2013) <http://www.anzspm.org.au/c/anzspm?
a=sendfile&ft=p&fid=1383782787>; Palliative Care Australia, Euthanasia and Physician Assisted Suicide (Position Statement, October 2011) <http://palliativecare.org.au/download/2448/> Australian Medical Association, The Role of the Medical Practitioner in End of Life Care 2007 (Position Statement, 5 September 2014) <https://ama.com.au/system/tdf/documents/ps_on_the_role_of_the_medical_
practitioner_in_end_of_life_care_2007_amended_2014_0.pdf?file=1&type=node&id=40572>; AMA Tasmania, AMA Tasmania’s Position on Euthanasia (March 2013) <https://ama.com.au/sites/default/
files/documents/2_-_AMA_Tasmania_submission_to_Consultation_Paper_on_Voluntary_Assisted_
Dying_draft_of_1st_March_2013.pdf>; The Royal Australian & New Zealand College of Psychiatrists, Physician Assisted Suicide (Position Statement, May 2011) <https://www.ranzcp.org/Files/Resources/
College_Statements/Position_Statements/ps67-pdf.aspx>; Australian Nursing Federation, Voluntary Euthanasia/Assisted Suicide (Position Statement, May 2012) <http://anmf.org.au/documents/policies/
PS_Voluntary_euthanasia.pdf>; Royal College of Nursing Australia, Position Statement: Voluntary Euthanasia/Assisted Suicide (Position Statement, 2006) <https://web.archive.org/web/20130430045203/
http://rcna.org.au/WCM/Images/RCNA_website/Files%20for%20upload%20and%20link/policy/documentation/position/voluntary_euthanasia.pdf>.
[75] Note that the recent Bill introduced by Liberal Democratic Party member, Senator David Leyonhjelm, is not included in the analysis in this section because the Bill is still before the Senate at the time of writing.
[77] B C Wright (ed), House of Representatives Practice (Department of the House of Representatives, 6th ed, 2012) 356; Robert Rogers and Rhodri Walters, How Parliament Works (Routledge, 6th ed, 2013) 208–9.
[78] Wright (ed), above n 77, 357.
[79] Ibid 361–3; Rogers and Walters, above n 77, 209–10.
[80] See, eg, Commonwealth, Parliamentary Debates, House of Representatives, 24 November 1920, 6906 (Elliot Johnson); Commonwealth, Parliamentary Debates, House of Representatives, 22 November 1932, 2601 (George Mackay).
[81] Wright (ed), above n 77, 374–5; Rogers and Walters, above n 77, 210–24.
[82] Wright (ed), above n 77, 376–7.
[83] Out of the 50 Bills analysed in Table 3, five were Bills seeking to facilitate a referendum on VE. Two of these Bills lapsed, and three were defeated.
[84] Wright (ed), above n 77, 296, 372–3.
[85] Ibid.
[86] Ibid.
[87] Rights of the Terminally Ill Bill 2003 (NSW).
[88] See, eg, Wright (ed), above n 77, 223–4, 228.
[89] Ibid 580.
[90] Ibid 573.
[91] Ibid.
[92] Ibid 861.
[93] See, eg, ibid 574–5.
[94] Ibid.
[95] South Australia, Parliamentary Debates, Legislative Council, 9 July 1997, 1783 (Sandra Kanck).
[96] Note that the recent Bill introduced by Liberal Democratic Party member, Senator David Leyonhjelm, is not included in the analysis in this section because the Bill is still before the Senate at the time of writing.
[97] For example, if there were 23 members in the relevant house, 12 members would need to support the Bill for it to be passed. A Bill would be regarded as ‘close to passing’ for the purpose of this article if 70 per cent or above of the 12 members supported the Bill.
[101] Sarah Edelman, ‘Politicians Out of Sync with Most Australians’ Views on Assisted Dying’, Sydney Morning Herald (online), 24 February 2015 <http://www.smh.com.au/comment/politicians-out-of-sync-with-most-australians-views-on-assisted-dying-20150224-13lzbh.html> . In a NSW election ABC Poll, of more than 34 000 respondents, 72 per cent strongly agreed or agreed with the proposition: ‘Terminally ill patients should be able to legally end their own lives with medical assistance’, compared with 16 per cent of respondents who did not and 11 per cent of who said they were neutral: Claire Aird, ‘NSW Election 2015: Almost Three Quarters of Voters Support Euthanasia, Vote Compass Finds’, ABC News (online), 15 March 2015 <http://www.abc.net.au/news/2015-03-15/nsw-voters-support-euthanasia-vote-compass-finds/6313864> . Polls of public views on euthanasia over the past 10 years have also indicated support for reform: 75 per cent in favour (The Australia Institute, Survey Results – Attitudes to Voluntary Euthanasia (6 January 2011) 2 <http://www.tai.org.au/downloadpopup/nojs/8589> ); 83.4 per cent in favour (Newspoll, Euthanasia Study (Job No 110302, March 2011) 8 <http://www.dwdnsw.org.au/
documents/2011/Newspoll%202011.pdf>); 84.9 per cent in favour (Newspoll survey cited in in AAP, ‘85 Per Cent Support Voluntary Euthanasia – Poll’, The Australian (online), 26 October 2009 <http://www.theaustralian.com.au/news/latest-news/per-cent-support-voluntary-euthanasia-poll/story-fn3dxiwe-1225791455181> ); 78 per cent in favour (Enterprise Marketing & Research Services Pty Ltd, Voluntary Euthanasia Research Report (May 2009) <http://tasmaniantimes.com/images/uploads/May24_
EMRS_V_Euthanasia_Poll_09_N_McKim_ATTACH.pdf>).
[102] The only observation that can be made regarding the likelihood of a particular kind of Bill to be successful or not is that the referendum Bills have never been ‘close to passing’ and appear to attract even less support than the defensive and permissive models. These models are discussed further in the following Part.
[103] The members of Parliament in SA (69), Tasmania (40) and NT (25) are small when compared with, eg, NSW (135), Victoria (128), WA (95) and Queensland (89).
[104] Plumb, above n 59, 72.
[105] Ibid 73–4.
[106] Ibid 73.
[107] Ibid 81.
[108] Timothy E Quill, Christine K Cassel and Diane E Meier, ‘Care for the Hopelessly Ill: Proposed Clinical Criteria for Physician Assisted Suicide’ (1992) 327 New England Journal of Medicine 1380, 1381; Margaret P Battin, ‘Euthanasia: The Way We Do It, the Way They Do It’ (1991) 6 Journal of Pain and Symptom Management 298, 300. A purported distinction between PAS and VE forms the foundation of the Oregon, Washington and Vermont Death with Dignity Acts (Or Rev Stat §§ 127.800–127.995 (1994); Wash Rev Code §§ 70.245.010–70.245.904 (2008); Vt Stat Ann §§ 5281–93 (2013)) which permit only PAS. For a discussion of arguments differentiating PAS from VE, see Nicholas Dixon, ‘On the Difference between Physician-Assisted Suicide and Active Euthanasia’ (1998) 28(5) Hastings Center Report 25. Most jurisdictions which have regulated PAS/VE practices, as illustrated in Part IV, draw no moral or legal distinction between VE and PAS.
[109] Voluntary Euthanasia Bill 2010 (WA) cl 11(1).
[110] While this may have merely been a drafting error, it is noted that each VE Bill introduced into the WA Parliament prior to 2010 either directly or indirectly contemplated self-administration by the patient: Voluntary Euthanasia Bill 1998 (WA) cl 8(5); Voluntary Euthanasia Bill 2000 (WA) cl 8(5); Voluntary Euthanasia Bill 2002 (WA) cl 8. The rationale for limiting permissible conduct to VE and not PAS is unclear. However, Robin Chapple, the proponent of the Bill, opened her second reading speech by stating that ‘[t]his Bill is not about legalising suicide’: Western Australia, Parliamentary Debates, Legislative Council, 20 May 2010, 3017 (Robin Chapple). Therefore, the decision to exclude PAS may have been a deliberate political choice to circumscribe any arguments that VE legislation effectively legalised or promoted suicide.
[111] After the passage of the Euthanasia Laws Act 1997 (Cth), Michael Moore from the ACT introduced the Crimes (Assisted Suicide) Bill 1997 (ACT). While this Bill was primarily crafted in terms of PAS, cls 5(d)(ii), (e)–(f) clearly contemplated the direct administration of lethal substances by the medical practitioner. Therefore, this was a mixed Bill.
[112] Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 5. In this context, ‘assistance’ includes giving information, prescribing, preparing or providing a drug, and providing assistance for the sufferer to ingest a drug, but does not include injection of lethal substances: at cl 3 (definition of ‘assistance’).
[113] ROTTIA s 4.
[114] ROTTIA s 3 (definition of ‘assist’).
[115] Rights of the Terminally Ill Bill 2001 (NSW) cl 3 (definition of ‘assist’); Dying with Dignity Bill 2009 (Tas) cl 3 (definition of ‘assist’).
[116] See, eg, Voluntary Euthanasia Bill 2002 (WA) cl 8; Voluntary Euthanasia Bill 2000 (WA) cl 8; Crimes (Assisted Suicide) Bill 2007 (ACT) cl 5.
[117] Voluntary Euthanasia Bill 2002 (WA) cl 8(2).
[118] Voluntary Euthanasia Bill 2012 (SA) cl 11(2).
[119] Lindy Willmott, Ben White and Shih-Ning Then, ‘Withholding and Withdrawing Life-Sustaining Medical Treatment’ in Ben White, Fiona McDonald and Lindy Willmott (eds), Health Law in Australia (Lawbook, 2nd ed, 2014) [14.20]–[14.40]. A competent patient is entitled to have a request for medical treatment to be withheld or withdrawn respected by his or her doctor: Brightwater Care Group Inc v Rossiter [2009] WASC 229; (2009) 40 WAR 84, 92 [32] (Martin CJ); Hunter and New England Area Health Service v A [2009] NSWSC 761; (2009) 74 NSWLR 88, 97 [40] (McDougall J). Legislation is therefore not required to enforce such a right.
[120] See, eg, McGee, ‘Does Withdrawing Life-Sustaining Treatment Cause Death’, above n 27; McGee, ‘Acting To Let Someone Die’, above n 27. See also John Keown who classifies the withholding or withdrawing of treatment as merely prudent medical practice where there is no intention to cause death: John Keown, ‘Against Decriminalising Euthanasia; For Improving Care’ in Emily Jackson and John Keown (eds), Debating Euthanasia (Hart Publishing, 2012) 83, 142–5.
[121] See, eg, Voluntary Euthanasia Bill 2012 (SA) cl 11.
[122] See, eg, Voluntary Euthanasia Bill 2012 (SA) cl 13.
[123] See, eg, Voluntary Euthanasia Bill 2012 (SA) cls 5–6.
[124] See, eg, Voluntary Euthanasia Bill 2012 (SA) cl 12.
[125] See, eg, Voluntary Euthanasia Bill 2012 (SA) cl 17. These provisions, however, vary in scope and operation: cf ROTTIA s 18.
[126] See, eg, Voluntary Euthanasia Bill 2012 (SA) cls 15, 19–20.
[127] Other examples include Rights of the Terminally Ill Bill 2001 (NSW); Voluntary Euthanasia Bill 2012 (SA); Dying with Dignity Bill 2009 (Tas); Medical Treatment (Physician Assisted Dying) Bill 2009 (Vic); Voluntary Euthanasia Bill 2010 (WA).
[128] See, eg, ROTTIA s 7(1)(c); Rights of the Terminally Ill Bill 2001 (NSW) cl 7(1)(c); Voluntary Euthanasia Bill 2006 (SA) cl 5(2); Dying with Dignity Bill 2001 (Tas) cl 8(1)(c); Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 5(m); Voluntary Euthanasia Bill 2000 (WA) cl 7(a).
[129] See, eg, ROTTIA s 7(1)(c); Right of the Terminally Ill Bill 2001 (NSW) cl 7(1)(g); Voluntary Euthanasia Bill 2007 (SA) cl 5(2); Voluntary Euthanasia Bill 2000 (WA) cl 7(b).
[130] See, eg, Voluntary Euthanasia Bill 2000 (WA) cl 7(b).
[131] See, eg, Rights of the Terminally Ill Bill 2001 (NSW) cl 7(e).
[132] See, eg, Voluntary Euthanasia Bill 2007 (SA) cl 5(3).
[133] ROTTIA s 7(1)(i).
[134] See, eg, ROTTIA s 7(1)(h).
[135] See, eg, ROTTIA ss 7(1)(i)–(j); Rights of the Terminally Ill Bill 2001 (NSW) cl 17; Voluntary Euthanasia Bill 2006 (SA) cl 7; Dying with Dignity Bill 2009 (Tas) cls 8(1)(j)–(k); Voluntary Euthanasia Bill 2010 (WA) cls 10–11.
[136] See generally South Australia, Parliamentary Debates, Legislative Assembly, 10 March 2011, 2849 (Stephanie Key); South Australia, Parliamentary Debates, Legislative Assembly, 28 July 2011, 4726 (Stephanie Key), where it was emphasised that the defensive model was a compromise designed to attain consensus on VE and PAS.
[137] See Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) s 13B(3).
[138] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) s 13B(1)(c).
[139] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) s 13B(1).
[140] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) s 13B(6)(a).
[141] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) ss 13B(1)(a), (2)(a).
[142] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) ss 13B(1)(b), (2)(b).
[143] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) ss 13B(1)(c), (2)(c).
[144] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) ss 13B(1)(d), (2)(d). Note that the proposed s 13B(5) expressly states that the court must have regard to parliament’s intention that it is reasonable to terminate a person’s life in exceptional circumstances where the medical condition causes their life to become irreversibly intolerable, including where palliative care cannot relieve the suffering to a level acceptable to the person.
[145] To be protected, the medical practitioner must have been duly acquitted under the defence provisions (the proposed s 13B(3)(a)), and the conduct of the person supporting or assisting was in good faith in the ordinary course of their employment and was a reasonable response to the person’s suffering (the proposed s 13B(3)(b)).
[146] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) ss 13B(1)–(3).
[147] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) s 13B(6)(a).
[148] The Bill was defeated resoundingly 3:14 (supported only by Michael Moore and the two Australian Greens members): Australian Capital Territory, Parliamentary Debates, Legislative Assembly, 5 November 1997, 3673. The Bill lost the support of two VE supporters, Wayne Berry and Simon Corbell, who regarded the Bill as ‘trivialising’ euthanasia: at 3656 (Wayne Berry); reinforcing opposing arguments by causing the pecuniary penalty to be less than a speeding ticket: at 3665 (Simon Corbell); and the associated concern of adverse media and public reactions: at 3656 (Wayne Berry). Another example of the penalty mitigation model is the Criminal Code (Euthanasia) Amendment Bill 1997 (NT) which imposed a $50 fine on medical practitioners performing VE subject to prescribed legislative criteria similar to that discussed under the Crimes (Assisted Suicide) Bill 1997 (ACT). See further Northern Territory, Parliamentary Debates, Legislative Assembly, 18 February 1998, 639–45 (John Bailey).
[149] Crimes (Assisted Suicide) Bill 1997 (ACT) cls 3 (definition of ‘request’), 5(a).
[150] Crimes (Assisted Suicide) Bill 1997 (ACT) cl 5(c).
[151] Crimes (Assisted Suicide) Bill 1997 (ACT) cl 5(b).
[152] Medical Treatment (Amendment) Bill 1995 (ACT); Rights of the Terminally Ill Bill 2011 (NSW). An extreme example of this model is the Death with Dignity Acts of three states in the United States (Or Rev Stat §§ 127.800–127.995 (1994); Wash Rev Code §§ 70.245.010–70.245.904 (2008); Vt Stat Ann §§ 5281–93 (2013)) which restrict PAS to only imminently lethal medical conditions by requiring the person to be in the terminal phase of a terminal illness and within six months of death.
[153] Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic); Rights of the Terminally Ill Bill 2001 (NSW); Consent to Medical Treatment and Palliative Care (Voluntary Euthanasia) Amendment Bill 2008 (SA).
[154] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) s 13B(1)(b).
[155] Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA) cl 3, inserting what would have been Criminal Law Consolidation Act 1935 (SA) s 13B(1)(b).
[156] We discuss when it is just pain, when it is pain and suffering, and when it is pain or suffering below. We also discuss the distinction between pain and suffering below. In the text, when we refer to ‘“pain” and “suffering”’, we are referring to these terms as they are used separately. By contrast, when we refer to ‘pain and suffering’, we are referring to that phrase as used in a statute, and as therefore embodying the requirement that there be both pain and suffering. The same considerations apply to the use of ‘“pain” or “suffering”’ and ‘pain or suffering’, though we shall also use ‘pain and/or suffering’ to signify these alternatives.
[157] Some important academic work by medical practitioners has been undertaken on the concept of suffering that it is outside the scope of the present article: see Eric J Cassel, ‘The Nature of Suffering and the Goals of Medicine’ (1982) 306 New England Journal of Medicine 639.
[158] See, eg, Rights of the Terminally Ill Bill 2001 (NSW) cl 4; ROTTIA s 4.
[159] See, eg, Medical Treatment (Amendment) Bill 1997 (ACT) cl 10, inserting what would have been Medical Treatment Act 1994 (ACT) ss 6A(d), 6B(2)(a)(ii).
[160] See, eg, Voluntary Euthanasia Bill 2006 (SA) cl 4(2)(b).
[161] As remedial or beneficial legislation, the courts may be more likely to adopt an expansive interpretation consistent with the objects of the legislation, namely providing a systematic framework enabling patients to terminate their suffering. See, eg, Wacal Developments Pty Ltd v Realty Developments Pty Ltd [1978] HCA 30; (1978) 140 CLR 503, 519–20 (Mason J); Minister Administering the Crown Lands Act v NSW Aboriginal Land Council (2008) 237 CLR 285, 290–3 [9]–[20] (Kirby J); Butler v Fife Coal Co Ltd [1911] UKLawRpAC 74; [1912] AC 149, 178–9 (Lord Shaw). On this basis, it is arguable that a more expansive interpretation of pain would be more appropriate.
[162] Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 3 (definition of ‘intolerable suffering’). The concept of ‘intolerable’ or ‘unbearable’ suffering is discussed in detail by H R W Pasman et al, ‘Concept of Unbearable Suffering in Context of Ungranted Requests for Euthanasia: Qualitative Interviews with Patients and Physicians’ (2009) 339 British Medical Journal 1235. The authors discuss the conflict between patients and doctors in understanding what ‘unbearable’ and ‘intolerable’ require.
[163] Medical Treatment and Palliative Care (Voluntary Euthanasia) Amendment Bill 2008 (SA) cl 19(1)(b)(ii).
[164] Rights of the Terminally Ill Bill 2011 (NSW) cl 7(f). However, other Bills, eg, Medical Treatment (Amendment) Bill 1995 (ACT), which require severe pain or distress, introduce subjective elements by specifying that it cannot be controlled by medical treatment to the person’s satisfaction.
[165] Voluntary Euthanasia Bill 2010 (WA) cl 6(1)(f)(i).
[166] Voluntary Euthanasia Bill 2012 (SA) cl 4(2)(b).
[167] Ibid.
[168] Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 3 (definition of ‘intolerable suffering’); Dying with Dignity Bill 2009 (Tas) cl 3 (definition of ‘intolerable suffering’). See also Medical Treatment and Palliative Care (Voluntary Euthanasia) Amendment Bill 2008 (SA) cl 19(1)(b)(ii).
[169] This is pursuant to its positioning in cl 7(1) of the Bill, which requires the medical practitioner to satisfy several elements prior to administering VE.
[170] Margo McCaffery, ‘Understanding Your Patient’s Pain Tolerance’ (1999) 29(12) Nursing 17, 17; G F Gebhart, ‘Pain’ in Marc D Binder, Nobutaka Hirokawa and Uwe Windhorst (eds), Encyclopedia of Neuroscience (Springer, 2009) 3063.
[171] Dying with Dignity Bill 2009 (Tas) cl 3 (definition of ‘intolerable suffering’); Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 3 (definition of ‘intolerable suffering’). There may be an ambiguity in the case of the latter Bill. The Bill required the treating doctor to be ‘satisfied on reasonable grounds that the sufferer has a terminal or incurable illness that is causing the sufferer intolerable suffering’: at cl 5(c). On the wording of the Bill, it could mean that the doctor must be reasonably satisfied that the patient has a terminal and incurable illness only, and not also reasonably satisfied that the terminal or incurable illness is causing the patient intolerable suffering (that being an issue that is only determinable by the patient himself or herself). Or it could mean that the doctor must be reasonably satisfied of both. On the first reading, ‘intolerable suffering’ is still given a subjective interpretation – what counts as ‘intolerable’ is determined exclusively by the patient. On the second interpretation, by contrast, ‘intolerable suffering’ must be given an objective meaning. Would a reasonable person in the patient’s position consider the suffering to be intolerable? The wording of the other clauses in the Bill suggest that only the former reading is intended – what counts as intolerable is to be judged by the patient.
[172] Voluntary Euthanasia Bill 2010 (WA) cl 6(1)(f)(i).
[173] See, eg, ROTTIA s 7(1)(i); Voluntary Euthanasia Bill 2012 (SA) cl 11(1)(f); Dying with Dignity Bill 2009 (Tas) cl 8(1)(n).
[174] ROTTIA s 8(1).
[175] The Voluntary Euthanasia Bill 1998 (WA) cl 4(2)(b) implies the existence of a relationship of proximity, similar to a causal relationship, through requiring the existence of pain, suffering or debilitation associated with the ‘actual progress of [the] illness or condition’.
[176] Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 5(c).
[177] Voluntary Euthanasia Bill 2010 (WA) cl 6(1)(f)(ii).
[178] The ‘but for’ test means that the illness would be the sole cause of the pain and/or suffering. The ‘material contribution test’ means that the illness would be one, but not the only, cause of the pain and/or suffering – there may be other causes as well, and it suffices that the illness only be one of them.
[179] See, eg, Rights of the Terminally Ill Bill 2001 (NSW) cl 4; ROTTIA s 4. See also, eg, Voluntary Euthanasia Bill 2012 (SA) cl 5; Dying with Dignity Bill 2009 (Tas) cl 5.
[180] Dignity in Dying Bill 2001 (SA) cl 6, introduced by Sandra Kanck; Dignity in Dying Bill 2001 (SA) cl 6, introduced by Bob Such; Dignity in Dying Bill 2002 (SA) cl 6; Dignity in Dying Bill 2003 (SA) cl 6(1)(b); Dignity in Dying Bill 2005 (SA) cl 6(1)(b). The primary safeguard in relation to the advance request is that the patient be informed of feasible VE procedures and the risks associated with them (see, eg, Dignity in Dying Bill 2005 (SA) cl 7(1)(c)), as well as in conjunction with witnessing and certification procedures (see, eg, Dignity in Dying Bill 2005 (SA) cls 8–9).
[181] See, eg, Medical Treatment (Amendment) Bill 1995 (ACT) cl 19, which would have amended Medical Treatment Act 1994 (ACT) s 13, provided that where an adult is of sound mind, and suffering severe pain in the terminal phase of a terminal illness, they may execute an instrument conferring on another person the power to request the administration of VE in the event that the patient becomes incapacitated.
[182] See, eg, Dying with Dignity Bill 2009 (Tas) cl 16(1); Voluntary Euthanasia Bill 2000 (WA) cl 11(1); Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 16; ROTTIA ss 14–15. Cf Voluntary Euthanasia Bill 2006 (SA) cl 19, which establishes the Voluntary Euthanasia Monitoring Committee.
[183] One Bill (2.6 per cent) can be categorised as the defence model (Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA)), and two Bills (5.1 per cent) have adopted the penalty mitigation model (Crimes (Assisted Suicide) Bill 1997 (ACT); Criminal Code (Euthanasia) Amendment Bill 1997 (NT)).The penalty mitigation models have only been introduced within the Australian territories immediately after the enactment of the Euthanasia Laws Act 1997 (Cth) to circumscribe its removal of legislative competency in respect of legalising or decriminalising VE or PAS.
[184] See, eg, Dignity in Dying Bill 2001 (SA) cl 6, introduced by Sandra Kanck; Dignity in Dying Bill 2001 (SA) cl 6, introduced by Bob Such; Dignity in Dying Bill 2002 (SA) cl 6; Dignity in Dying Bill 2003 (SA) cl 6(1)(b); Dignity in Dying Bill 2005 (SA) cl 6(1)(b).
[185] See, eg, Medical Treatment (Amendment) Bill 1995 (ACT) cl 19, which would have amended Medical Treatment Act 1994 (ACT) s 13.
[186] See, eg, Voluntary Euthanasia Bill 2012 (SA) s 4(2)(b); Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 3 (definition of ‘intolerable suffering’); Dying with Dignity Bill 2009 (Tas) cl 3 (definition of ‘intolerable suffering’).
[187] For broad definitions of the concept of suffering see, eg, Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 3; Medical Treatment and Palliative Care (Voluntary Euthanasia) Amendment Bill 2008 (SA) cl 19(1); Rights of the Terminally Ill Bill 2001 (NSW) cl 4; ROTTIA s 4. However, as noted above, where pain is used on its own, it may well be given an equally broad interpretation. When used alongside ‘suffering’, it may be restricted to physical pain, but the addition of the word suffering will mean that the definition is broad unless the terms appear conjunctively, which would limit the circumstances of suffering to suffering associated with physical pain.
[188] See, eg, Voluntary Euthanasia Bill 2007 (SA) cl 5(3); Rights of the Terminally Ill Bill 2001 (NSW) cl 7(1)(e).
[189] See, eg, ROTTIA s 7(1)(c)(iv).
[190] See, eg, ROTTIA s 7(1)(h).
[191] See, eg, Voluntary Euthanasia Bill 2006 (SA) cl 7; ROTTIA ss 7(1)(i)–(j); Dying with Dignity Bill 2009 (Tas) cls 8(1)(i)–(j).
[192] See, eg, ROTTIA s 7(1)(i); Voluntary Euthanasia Bill 2000 (WA) cl 8(3); Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 5(o).
[193] See, eg, Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 5(b); Dying with Dignity Bill 2009 (Tas) cl 9.
[194] See, eg, Dying with Dignity Bill 2009 (Tas) cl 16(1); Voluntary Euthanasia Bill 2000 (WA) cl 11(1); Medical Treatment (Physician Assisted Dying) Bill 2008 (Vic) cl 16; ROTTIA ss 14–15. Cf Voluntary Euthanasia Bill 2006 (SA) s 19, which establishes the Voluntary Euthanasia Monitoring Committee.
[195] Dignity in Dying Bill 2001 (SA); Consent to Medical Treatment and Palliative Care (Voluntary Euthanasia) Amendment Bill 2008 (SA).
[196] By contrast, could it be argued that, within SA, a Bill that is broader has a greater chance of passing than a Bill that is narrower? No, for there are SA Bills with the same requirements that were not close to passing, such as the Criminal Law Consolidation (Medical Defences – End of Life Arrangements) Amendment Bill 2011 (SA).
[197] See, eg, Bregje D Onwuteaka-Philipsen et al, ‘Trends in End-of-Life Practices before and after the Enactment of the Euthanasia Law in the Netherlands from 1990 to 2010: A Repeated Cross-sectional Survey’ (2012) 380 The Lancet 908; Kenneth Chambaere et al, ‘Trends in Medical End-of-Life Decision Making in Flanders, Belgium: 1998–2001–2007’ (2011) Medical Decision Making 500; Kenneth Chambaere et al, ‘Physician-Assisted Deaths under the Euthanasia Law in Belgium: A Population-Based Survey’ (2010) 182 Canadian Medical Association Journal 895; Luc Deliens et al, ‘End-of-Life Decisions in Medical Practice in Flanders, Belgium: A Nationwide Survey’ (2000) 356 The Lancet 1806; Paul van der Maas et al, ‘Euthanasia, Physician-Assisted Suicide, and Other Medical Practices Involving the End of Life in the Netherlands, 1990–1995’ (1996) 335 New England Journal of Medicine 1699; Paul J van der Mass, ‘Euthanasia and Other Medical Decisions Concerning the End of Life’ (1991) 338 The Lancet 669.
[198] This table expands a similar table included in White and Willmott, above n 2.
AustLII:
Copyright Policy
|
Disclaimers
|
Privacy Policy
|
Feedback
URL: http://www.austlii.edu.au/au/journals/UNSWLawJl/2016/1.html